Bronze Diabetes: Exploration of Hemochromatosis-Associated Diabetes Mellitus
Bronze diabetes, also known as bronze diabetes mellitus, is a unique form of diabetes arising from the underlying condition known as hemochromatosis. This comprehensive article aims to provide an in-depth exploration of bronze diabetes, including its pathophysiology, clinical manifestations, diagnosis, and management strategies. With a detailed analysis of the relationship between hemochromatosis and diabetes and the impact of iron overload on pancreatic Function, this article seeks to enhance understanding and awareness of this rare and complex condition.
Introduction to Bronze Diabetes
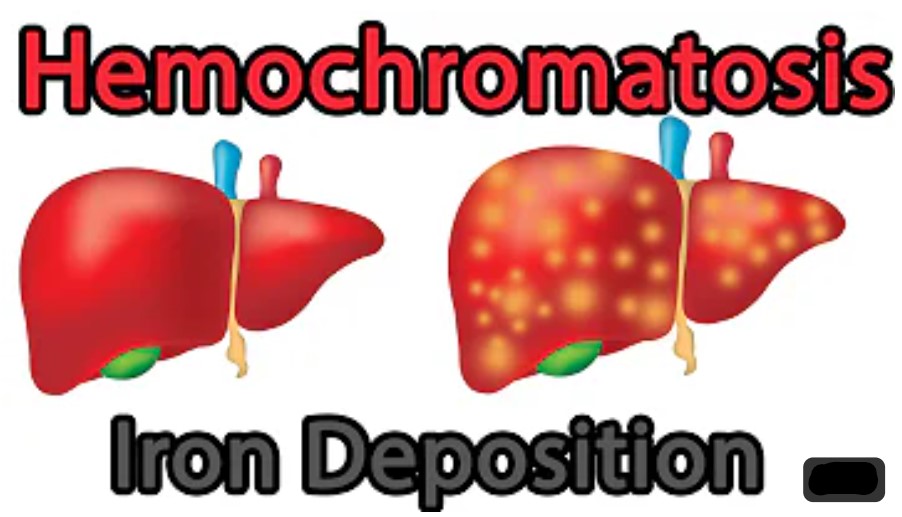
Bronze diabetes is a medical condition known as hemochromatosis. Hemochromatosis is a genetic disorder that causes the body to absorb and store too much iron, leading to iron buildup in various organs such as the liver, pancreas, and heart. Over time, this excess iron can cause damage to these organs and lead to various complications.
Suppose someone with hemochromatosis develops diabetes due to the excess iron buildup in their pancreas. In that case, it is called “bronze diabetes” because the iron buildup can cause a bronzed skin tone. However, this is not a medical term commonly used in healthcare.
Overview of bronze diabetes
Bronze diabetes is a genetic disorder in which the body absorbs and stores too much iron from the diet. This excess iron accumulation can damage several organs, including the liver, heart, and pancreas. In the pancreas, the iron buildup can cause damage to the insulin-producing cells, resulting in diabetes.
When someone with hemochromatosis develops diabetes due to iron buildup in their pancreas, it may result in a bronzed skin tone, particularly in the face, neck, and hands. This discolouration is caused by the accumulation of iron in the skin cells.
Explanation of the term “bronze” concerning the condition
The term “bronze” is used concerning the discoloration of the skin that can occur in individuals with hemochromatosis-related diabetes. Iron accumulation in the skin cells can cause a bronzed or brownish-gray color on the face, neck, and hands. This is known as hyperpigmentation.
The exact mechanism behind the hyperpigmentation has yet to be fully understood. Still, it is thought to be due to the deposition of melanin, a pigment that gives colour to the skin, in response to iron overload. In addition, the iron buildup may also damage the skin cells, further contributing to discolouration.
It is important to note that not all individuals with hemochromatosis-related diabetes will develop bronze skin. Hyperpigmentation is a rare and late manifestation of the condition and typically occurs in individuals with long-standing and severe iron overload. Therefore, the absence of skin discolouration does not rule out the presence of hemochromatosis or hemochromatosis-related diabetes.
Introduction to hemochromatosis as the underlying cause of Bronze diabetes
Hemochromatosis is a genetic disorder that causes the body to absorb and store too much iron from the diet. This excess iron accumulation can damage several organs, including the liver, heart, and pancreas. In the pancreas, the iron buildup can cause damage to the insulin-producing cells, resulting in diabetes.
There are two types of hemochromatosis: primary and secondary. Primary hemochromatosis is the most common form and is caused by a genetic mutation that results in increased iron absorption from the diet. Secondary hemochromatosis can occur due to other medical conditions, such as chronic liver disease, thalassemia, or frequent blood transfusions.
Hemochromatosis-related diabetes, also known as “bronze diabetes,” occurs when the iron buildup in the pancreas damages the insulin-producing cells, resulting in diabetes. The term “bronze diabetes” refers to the hyperpigmentation or bronzed skin tone that can occur in individuals with this condition due to iron accumulation in the skin cells.
Diagnosis of hemochromatosis is typically made through blood tests that measure iron levels and other iron overload markers. Treatment involves managing the excess iron levels in the body through phlebotomy (bloodletting) or chelation therapy. In individuals with hemochromatosis-related diabetes, controlling blood sugar levels with medication and lifestyle changes is vital to prevent complications. Early diagnosis and treatment are crucial to prevent further organ damage and improve outcomes.
Significance of early detection and management
Early detection and management of hemochromatosis and hemochromatosis-related diabetes are crucial to prevent complications and improve outcomes. If left untreated, the excess iron accumulation in various organs can cause severe damage and life-threatening conditions.
In the liver, hemochromatosis can cause cirrhosis, liver cancer, and liver failure. In the heart, it can lead to heart failure and arrhythmias. In the pancreas, it can cause damage to the insulin-producing cells, leading to diabetes. In addition, excess iron in the body can also cause joint pain, skin discolouration, and sexual dysfunction.
Early detection and treatment of hemochromatosis can prevent or delay the development of these complications. Phlebotomy, a procedure in which blood is removed from the body to reduce iron levels, is the most common treatment for hemochromatosis. Chelation therapy, which involves medication to bind and remove excess iron, may also be used in some cases.
Controlling blood sugar levels is crucial in individuals with hemochromatosis-related diabetes. Lifestyle changes, such as a healthy diet and regular exercise, can also help to manage blood sugar levels and prevent complications.
Early detection and management of hemochromatosis and hemochromatosis-related diabetes can improve outcomes and prevent serious complications. Discuss screening and management options with your healthcare provider if you are concerned about developing these conditions.
Hemochromatosis: Causes and Pathophysiology
Hemochromatosis is a genetic disorder characterized by increased absorption and iron accumulation in the body. It is caused by mutations in one or more genes that regulate iron metabolism. Mutations in the HFE gene cause the most common form of hemochromatosis.
Typically, the body regulates the amount of iron absorbed from the diet. Iron is essential to produce red blood cells, but excess iron can be toxic and damage organs. In individuals with hemochromatosis, the regulation of iron absorption is disrupted, leading to excessive accumulation of iron in various organs such as the liver, pancreas, heart, and joints.
The excess iron in these organs can cause damage through several mechanisms. One of the main mechanisms is oxidative stress. Iron can participate in reactions that generate reactive oxygen species (ROS), harmful molecules that can damage DNA, proteins, and other cellular structures. ROS can cause inflammation and cell death, leading to organ damage.
In the liver, excess iron can cause liver damage and cirrhosis, which can progress to liver failure and cancer. In the pancreas, excess iron can cause damage to the insulin-producing cells, leading to diabetes. In the heart, excess iron can cause heart failure and arrhythmias. In the joints, excess iron can cause pain and inflammation.
The symptoms of hemochromatosis can vary widely and may include fatigue, joint pain, abdominal pain, and sexual dysfunction. However, many individuals with hemochromatosis do not have any symptoms, and the condition may only be detected through routine blood tests that show increased iron levels.
Hemochromatosis is a complex disorder with multiple causes and mechanisms of disease. The underlying genetic mutations disrupt iron metabolism, accumulating iron in various organs and causing long-term complications.
Definition and classification of hemochromatosis
Hemochromatosis is a genetic disorder characterized by excessive iron accumulation in the body. Iron is a crucial nutrient that plays a vital role in many bodily functions, including the formation of red blood cells. However, when there is an excessive amount of iron, it can lead to damage to vital organs such as the liver, heart, and pancreas.
There are two main types of hemochromatosis:
- Primary hemochromatosis: This is also known as hereditary hemochromatosis and is caused by genetic mutations that affect how the body processes iron. It is the most common form of hemochromatosis, typically diagnosed in middle age.
- Secondary hemochromatosis: This type of hemochromatosis is caused by other medical conditions such as chronic liver disease, thalassemia, or anaemia that require frequent blood transfusions. Secondary hemochromatosis can also occur due to excessive iron intake through diet or supplements.
Hemochromatosis can be further classified into four subtypes based on the genetic mutations that cause the disorder:
- Type 1 hemochromatosis: is the most common form of hemochromatosis and is caused by mutations in the HFE gene.
- Type 2 hemochromatosis: This is caused by mutations in the HAMP, HJV, and HFE2 genes.
- Type 3 hemochromatosis: This is caused by mutations in the TFR2 gene.
- Type 4 hemochromatosis: This is caused by mutations in the SLC40A1 gene.
It’s important to note that not everyone with these genetic mutations will develop hemochromatosis, and some may develop the disorder without any of these mutations. Diagnosis is typically made through a blood test to measure iron levels and genetic testing to look for mutations associated with hemochromatosis. Treatment may involve regular blood removal (phlebotomy) to reduce iron levels, medications to help remove excess iron, and dietary changes to limit iron intake.
Genetic and acquired factors contributing to iron overload
Iron overload, or excess iron accumulation in the body, can result from genetic and acquired factors.
Genetic factors
The most common genetic cause of iron overload is hereditary hemochromatosis, a condition in which gene mutations that regulate iron metabolism cause excessive iron absorption and accumulation. The HFE gene is the most commonly mutated in hereditary hemochromatosis. Other rare genetic disorders that can cause iron overload include African iron overload, aceruloplasminemia, and ferroportin disease.
Acquired factors
Iron overload can also be acquired through various medical conditions or behaviours. Some examples include:
- Chronic liver disease can cause iron accumulation in the liver due to impaired Function of hepatocytes responsible for storing iron.
- Blood transfusions: Repeated blood transfusions can lead to iron overload in individuals with thalassemia or sickle cell disease.
- Excessive iron supplementation: Taking high iron supplements can lead to iron overload.
- Alcoholism: Chronic alcohol consumption can lead to liver damage and impaired iron metabolism, leading to iron overload.
- Other medical conditions: Certain conditions, such as chronic kidney disease, hypopituitarism, and some types of anaemia, can cause iron overload.
The symptoms of iron overload can vary and may include fatigue, joint pain, abdominal pain, and skin discolouration. Over time, iron overload can lead to severe complications such as cirrhosis, heart failure, and diabetes.
Treatment for iron overload typically involves removing excess iron from the body through regular phlebotomy (bloodletting) or chelation therapy, which involves using medications to bind and remove excess iron. Management of the underlying cause of iron overload is also essential to prevent further iron accumulation.
Explanation of iron metabolism and its dysregulation in hemochromatosis
Iron is vital for many biological processes, including oxygen transport, DNA synthesis, and electron transport in the respiratory chain. However, excess iron can lead to oxidative damage and tissue injury, making iron homeostasis a tightly regulated process in the body.
Several proteins regulate iron metabolism, including transferrin, ferritin, and hepcidin. Transferrin is a protein that binds to iron and transports it to cells throughout the body. Ferritin is a protein that stores excess iron in cells and releases it when needed. Hepcidin is a hormone produced in the liver that controls iron absorption by binding to and degrading the iron transporter ferroportin, thereby reducing the amount of iron that can be absorbed from the diet.
Hemochromatosis is a genetic disorder that leads to iron accumulation in the body, causing tissue damage and organ dysfunction. Hemochromatosis can be caused by mutations in several genes, including HFE, which regulates hepcidin production. In most cases of hereditary hemochromatosis, a mutation in the HFE gene results in decreased hepcidin production and increased iron absorption, leading to iron overload in the body.
Iron overload in hemochromatosis can lead to various symptoms, including fatigue, joint pain, abdominal pain, and liver disease. Iron overload can also increase the risk of developing diabetes, heart disease, and certain cancers. Treatment for hemochromatosis usually involves regular phlebotomy, which involves removing blood from the body to reduce iron levels, as well as dietary changes to reduce iron intake.
Iron metabolism is a complex process tightly regulated in the body. Hemochromatosis is a genetic disorder that results in iron accumulation in the body, leading to tissue damage and organ dysfunction. The dysregulation of iron metabolism in hemochromatosis is usually caused by gene mutations in regulating hepcidin production and iron absorption.
Role of the HFE gene mutation in hereditary hemochromatosis
The HFE gene mutation plays a critical role in hereditary hemochromatosis, a genetic disorder characterized by excessive absorption and iron accumulation in the body. The HFE gene provides instructions for making a protein that helps regulate the amount of iron absorbed from food.
In hereditary hemochromatosis, mutations in the HFE gene cause the body to absorb too much iron, leading to iron overload. The most common mutations associated with hereditary hemochromatosis are C282Y and H63D.
Individuals with two copies of the C282Y mutation are at the highest risk of developing iron overload, while those with one copy of C282Y and one copy of H63D or two copies of H63D are at lower risk. However, not all individuals with HFE mutations develop hemochromatosis, suggesting other factors may affect disease development.
Early symptoms of hereditary hemochromatosis can be vague and may include fatigue, joint pain, and abdominal pain. If left untreated, iron overload can cause serious complications such as liver disease, diabetes, and heart failure. Treatment for hereditary hemochromatosis typically involves regular blood removal (phlebotomy) to reduce iron levels and prevent complications.
Bronze Diabetes: Understanding the Relationship
Bronze diabetes, also known as hemochromatosis-related diabetes, is a rare but serious condition that occurs when excess iron accumulates in the body, leading to both diabetes and a bronze or greyish-brown discolouration of the skin. This condition is typically caused by a genetic mutation that affects the body’s ability to regulate iron absorption and storage.
The relationship between bronze diabetes and diabetes is complex. Still, excess iron in the body can damage the insulin-producing cells in the pancreas, leading to a reduction in insulin production and an increased risk of developing diabetes. Additionally, excess iron can cause insulin resistance, making it more difficult for the body to use insulin effectively and leading to diabetes.
Bronze diabetes is typically diagnosed through blood tests that measure iron levels. Treatment typically involves regular blood removal (phlebotomy) to reduce iron levels, along with the management of diabetes through diet, exercise, and medication.
It’s important to note that while bronze diabetes is a rare condition, it can have serious health consequences if left untreated, including liver damage, heart disease, and even death. If you have a family history of hemochromatosis or experience symptoms such as fatigue, joint pain, or abdominal pain, talk to your healthcare provider about getting tested for this condition.
Explanation of how iron overload leads to pancreatic dysfunction
Iron overload, or hemochromatosis, is a medical condition characterized by excess iron accumulation in the body’s tissues and organs. While iron is an essential mineral required for various physiological processes, too much iron can be toxic and lead to tissue damage and dysfunction.
The pancreas is an organ in the abdomen that plays a vital role in digestion and glucose metabolism. Iron overload can affect the pancreas in several ways, leading to pancreatic dysfunction.
Iron overload can damage the pancreas by directly damaging the pancreatic cells. Excess iron can accumulate in the pancreatic cells, leading to oxidative stress and cellular damage. This damage can impair the Function of the pancreatic cells, leading to decreased insulin secretion and impaired glucose metabolism.
Another way iron overload can affect the pancreas is by disrupting the hormonal regulation of glucose metabolism. Iron overload can lead to increased hepcidin levels, a hormone that regulates iron metabolism. Elevated hepcidin levels can impair the Function of pancreatic beta cells, which are responsible for producing insulin, leading to decreased insulin secretion and impaired glucose metabolism.
Iron overload can also increase the risk of developing diabetes mellitus. Excess iron can impair glucose tolerance and sensitivity, leading to insulin resistance and type 2 diabetes mellitus.
Iron overload can lead to pancreatic dysfunction through direct damage to pancreatic cells, disruption of hormonal regulation, and increased risk of developing diabetes mellitus. Diagnosing and managing iron overload is important to prevent or mitigate its effects on pancreatic Function.
Impact of iron deposition on beta-cell Function and insulin secretion
Iron deposition can have a significant impact on beta-cell Function and insulin secretion. Excess iron in the body can lead to iron overload or hemochromatosis, resulting in various complications, including diabetes mellitus.
Iron overload can cause damage to beta cells, which are responsible for producing insulin in the pancreas. This damage can lead to decreased beta-cell mass and impaired insulin secretion. Iron overload can also lead to oxidative stress, inflammation, and apoptosis (programmed cell death) of beta cells, which further exacerbates the damage to these cells.
Studies have shown that iron overload can impair glucose-stimulated insulin secretion and decrease insulin sensitivity. This can lead to impaired glucose tolerance and, ultimately, the development of type 2 diabetes. In addition, iron overload can also lead to the development of other complications associated with diabetes, such as cardiovascular disease, neuropathy, and retinopathy.
Therefore, it is important to monitor iron levels in individuals at risk for iron overload and hemochromatosis and to manage this condition appropriately to prevent or manage diabetes and other related complications.
Comparison of bronze diabetes with other types of diabetes (type 1 and type 2)
Bronze diabetes, also known as hemochromatosis-related diabetes or diabetes secondary to hemochromatosis, is a rare form of diabetes caused by an excess of iron in the body. This excess iron can damage the pancreas, the organ responsible for producing insulin, leading to diabetes.
Here are some key differences between bronze diabetes and type 1 and type 2 diabetes:
- Cause: Bronze diabetes is caused by hemochromatosis, a genetic disorder that causes the body to absorb too much iron. In contrast, type 1 diabetes is an autoimmune disorder in which the immune system attacks and destroys the insulin-producing cells in the pancreas, and type 2 diabetes is caused by a combination of genetic and lifestyle factors, such as obesity, physical inactivity, and poor diet.
- Age of onset: Bronze diabetes typically develops in adulthood, type 1 diabetes often develops in childhood or adolescence, and type 2 diabetes typically develops in middle age or later.
- Insulin production: In bronze diabetes, excess iron may damage the pancreas, decreasing insulin production. In type 1 diabetes, there is a complete lack of insulin production due to the destruction of the insulin-producing cells. In type 2 diabetes, the body becomes resistant to insulin, and the pancreas may eventually produce less insulin over time.
- Treatment: Bronze diabetes is typically treated by managing the underlying hemochromatosis, such as by regular phlebotomies to remove excess iron from the body. Type 1 diabetes is treated with insulin therapy, while type 2 diabetes may be treated with lifestyle changes, oral medications, and insulin therapy, depending on the severity of the condition.
- Prevalence: Bronze diabetes is a rare form of diabetes, accounting for less than 1% of all cases. Type 1 diabetes accounts for approximately 5-10% of all diabetes cases, while type 2 diabetes accounts for most cases (around 90-95%).
In summary, while all three types of diabetes involve abnormal glucose metabolism, the causes, age of onset, insulin production, treatment, and prevalence of bronze diabetes differ from those of type 1 and type 2 diabetes.
Prevalence and incidence of bronze diabetes in hemochromatosis patients
Bronze diabetes, also known as diabetes secondary to hemochromatosis, is a rare form of diabetes caused by excess iron accumulation in the pancreas. Hemochromatosis is an inherited disorder that affects approximately 1 in 200 to 1 in 300 individuals of European descent, making it one of this population’s most common genetic disorders.
The prevalence and incidence of bronze diabetes in hemochromatosis patients are not well established due to its rarity and the difficulty in diagnosing it. However, some studies have reported that up to 40% of patients with hemochromatosis may develop diabetes, although not all of these cases are necessarily caused by excess iron deposition in the pancreas.
It is important to note that not all individuals with hemochromatosis will develop diabetes, and other factors, such as age, gender, and lifestyle, may influence the risk of developing diabetes. Regular monitoring and screening for diabetes are recommended for individuals with hemochromatosis, especially those with a family history of diabetes or other risk factors.
In summary, while the prevalence and incidence of bronze diabetes in hemochromatosis patients are not well established, studies suggest that a significant proportion of patients with hemochromatosis may develop diabetes, and regular monitoring and screening for the disease are important in this population.
Clinical Manifestations of Bronze Diabetes
Bronze diabetes, also known as hemochromatosis-related diabetes, is a rare condition due to excessive iron accumulation in the body. This can lead to a range of clinical manifestations, including:
- Diabetes mellitus: The most common symptom of bronze diabetes is diabetes mellitus, characterized by high blood sugar levels. Symptoms of diabetes mellitus can include frequent urination, increased thirst, blurry vision, fatigue, and slow-healing wounds.
- Skin pigmentation: Another characteristic symptom of bronze diabetes is skin pigmentation. The skin may take on a bronze or grey colour due to the accumulation of iron in the skin.
- Joint pain: Hemochromatosis can cause joint pain and swelling, particularly in the knuckles of the fingers.
- Liver damage: Hemochromatosis can cause liver damage and cirrhosis in severe cases.
- Cardiomyopathy: Iron accumulation in the heart can lead to cardiomyopathy, a condition where the heart muscle becomes weakened and enlarged.
- Hypogonadism: In men, hemochromatosis can cause hypogonadism, a condition where the testes do not produce enough testosterone. This can lead to decreased libido, impotence, and infertility.
- Thyroid dysfunction: Hemochromatosis can also cause thyroid dysfunction, leading to fatigue, weight gain, and depression.
It is important to note that not all individuals with bronze diabetes will experience all of these symptoms. The severity and presentation of symptoms can vary widely among individuals with this condition. Treatment for bronze diabetes typically involves managing blood sugar levels through diet, exercise, and medication and managing iron levels through regular phlebotomy or iron chelation therapy.
Overview of the clinical features and symptoms of bronze diabetes
Bronze diabetes, also known as hemochromatosis-related diabetes, is a rare condition due to excessive iron accumulation in the body. This can lead to a range of clinical features and symptoms, including:
- Skin pigmentation: The skin may take on a bronze or grey colour due to the accumulation of iron in the skin.
- Diabetes mellitus: The most common symptom of bronze diabetes is diabetes mellitus, characterized by high blood sugar levels. Symptoms of diabetes mellitus can include frequent urination, increased thirst, blurry vision, fatigue, and slow-healing wounds.
- Joint pain: Hemochromatosis can cause joint pain and swelling, particularly in the knuckles of the fingers.
- Fatigue: Excessive iron accumulation in the body can cause fatigue and weakness.
- Liver damage: Hemochromatosis can cause liver damage and cirrhosis in severe cases.
- Cardiomyopathy: Iron accumulation in the heart can lead to cardiomyopathy, a condition where the heart muscle becomes weakened and enlarged.
- Hypogonadism: In men, hemochromatosis can cause hypogonadism, a condition where the testes do not produce enough testosterone. hemochromatosis
- It can lead to decreased libido, impotence, and infertility.
- Thyroid dysfunction: Hemochromatosis can also cause thyroid dysfunction, leading to fatigue, weight gain, and depression.
It is important to note that not all individuals with bronze diabetes will experience all of these symptoms. The severity and presentation of symptoms can vary widely among individuals with this condition. Treatment for bronze diabetes typically involves managing blood sugar levels through diet, exercise, and medication and managing iron levels through regular phlebotomy or iron chelation therapy. Early diagnosis and treatment can help prevent complications and improve outcomes for individuals with bronze diabetes.
Analysis of the bronze or greyish-brown skin pigmentation
The bronze or greyish-brown skin pigmentation in individuals with bronze diabetes results from the excessive accumulation of iron in the skin, which can cause the skin to take on a characteristic hue. This skin pigmentation is commonly seen on the face, neck, and hands and can be a useful diagnostic sign for healthcare providers.
The skin pigmentation is typically diffuse, symmetrical, and most prominent on sun-exposed areas of the skin. It can range in colour from light brown to deep bronze or grey. In some cases, the pigmentation may be patchy or irregular.
The skin pigmentation in bronze diabetes is thought to be due to the accumulation of iron in the melanin-producing cells of the skin, known as melanocytes. The excess iron can interfere with the production and distribution of melanin, leading to characteristic skin colour changes.
Not all individuals with bronze diabetes will experience skin pigmentation changes, and the severity and presentation of skin pigmentation can vary widely among affected individuals. The skin pigmentation in bronze diabetes is typically irreversible, but treatment for the underlying condition can help prevent further progression of the pigmentation and other complications associated with the disease.
Association with other complications of hemochromatosis, such as liver disease and cardiomyopathy
Bronze diabetes, which is a type of diabetes that occurs as a complication of hemochromatosis, can be associated with other complications of the disease, such as liver disease and cardiomyopathy.
Hemochromatosis is a genetic disorder that causes the body to absorb and store too much iron, leading to iron overload. Over time, this excess iron can cause damage to various organs, including the liver and heart.
Liver disease is a common complication of hemochromatosis and can range in severity from mild liver enzyme abnormalities to severe liver damage and cirrhosis. Iron overload can cause inflammation and liver cell damage, eventually leading to fibrosis and cirrhosis if left untreated. Symptoms of liver disease in hemochromatosis can include fatigue, abdominal pain, and jaundice.
Cardiomyopathy, or heart muscle disease, is another potential complication of hemochromatosis. Iron overload in the heart can lead to cardiomyopathy, which can cause symptoms such as shortness of breath, fatigue, and swelling of the legs and ankles. In severe cases, cardiomyopathy can lead to heart failure, arrhythmias, and sudden death.
Managing hemochromatosis-related complications typically involves reducing the iron overload in the body through regular phlebotomy (blood removal) or iron chelation therapy (medications that help remove excess iron from the body). Early diagnosis and treatment can help prevent or slow the progression of these complications and improve outcomes for individuals with hemochromatosis.
Identifying risk factors for developing bronze diabetes
Bronze diabetes, also known as hemochromatosis-related diabetes, is a rare condition due to excessive iron accumulation in the body. While the underlying cause of hemochromatosis is genetic, certain risk factors can increase an individual’s likelihood of developing the condition and, subsequently, bronze diabetes.
Some potential risk factors for developing hemochromatosis and bronze diabetes include:
- Family history: Hemochromatosis is an inherited condition, and individuals with a family history of the disease are at increased risk of developing the condition.
- Ethnicity: Hemochromatosis is more common in individuals of Northern European descent, although the condition can occur in individuals of any ethnicity.
- Age: Hemochromatosis is typically diagnosed in individuals over 30, although the condition can develop at any age.
- Gender: Hemochromatosis is more common in men than women, although women can still develop the condition.
- Alcohol consumption: Chronic alcohol consumption can increase the risk of developing hemochromatosis and exacerbate iron overload’s effects.
- Hepatitis C infection: Hepatitis C infection can also increase the risk of developing hemochromatosis.
- Iron-rich diet: A diet high in iron-rich foods can contribute to iron overload in susceptible individuals.
It is important to note that not all individuals with these risk factors will develop hemochromatosis or bronze diabetes. However, individuals with these risk factors should discuss the possibility of screening for hemochromatosis with their healthcare provider. Early detection and treatment can help prevent or slow the progression of complications associated with the disease.
Diagnosis of Bronze Diabetes
Bronze diabetes is another name for hemochromatosis, a genetic disorder that affects how the body metabolizes iron. The term “bronze diabetes” is used because individuals with hemochromatosis may have a bronze-like skin colour and symptoms similar to diabetes.
Diagnosing hemochromatosis typically involves a combination of medical history, physical examination, and laboratory tests. The following are some of the methods that may be used in the diagnosis of hemochromatosis:
- Medical history: The doctor may ask questions about symptoms, family history, and other medical conditions that the individual may have.
- Physical examination: The doctor may look for signs of bronze skin colouration, joint pain, liver enlargement, or other symptoms of hemochromatosis.
- Blood tests: Blood tests can measure the amount of iron in the blood and other markers of iron metabolism. The doctor may also check the levels of liver enzymes and ferritin, a protein that binds and stores iron.
- Genetic testing: Genetic testing can confirm the presence of the mutations that cause hemochromatosis.
If hemochromatosis is diagnosed, treatment may involve:
- Phlebotomy (removal of blood to reduce iron levels).
- Chelation therapy (medications that bind to excess iron).
- Changes in diet and lifestyle.
Working closely with a healthcare provider to manage the condition and prevent complications is important.
Diagnostic criteria and guidelines for hemochromatosis and bronze diabetes
The diagnostic criteria and guidelines for hemochromatosis (bronze diabetes) vary depending on the organization or medical association. However, the following are some common criteria and guidelines used for the diagnosis of hemochromatosis:
- Clinical criteria: Clinical symptoms, such as fatigue, joint pain, and liver disease, in addition to increased serum iron and ferritin levels.
- Laboratory criteria: Elevated serum iron and ferritin levels, low transferrin saturation, and elevated liver enzymes.
- Genetic testing: The presence of homozygous mutations in the HFE gene (C282Y/C282Y or C282Y/H63D) or compound heterozygosity for HFE mutations (C282Y/H63D, C282Y/S65C, or H63D/S65C) in individuals with elevated serum iron or ferritin levels.
- Family screening: Screening first-degree relatives of individuals with hemochromatosis using serum iron and ferritin levels, transferrin saturation, and genetic testing.
It is important to note that not all individuals with high serum iron or ferritin levels have hemochromatosis. A healthcare provider should make the diagnosis with experience in managing this condition. Additionally, the treatment and management of hemochromatosis should be tailored to the individual’s specific needs and medical history.
Role of laboratory tests in Detecting iron overload and pancreatic dysfunction
Laboratory tests play a critical role in detecting iron overload and pancreatic dysfunction.
Iron Overload: One of the most common laboratory tests for iron overload is serum ferritin level. Ferritin is a protein that stores iron in cells, and a high serum ferritin level is a marker of iron overload. Other laboratory tests that may diagnose iron overload include transferrin saturation and total iron-binding capacity (TIBC) tests. These tests measure the amount of iron bound to transferrin, a protein that carries iron in the blood, and the amount of transferrin available to bind iron.
Pancreatic Dysfunction: Laboratory tests can also be used to detect pancreatic dysfunction. The most common laboratory tests for pancreatic Function are blood tests that measure levels of pancreatic enzymes, such as amylase and lipase. The pancreas normally produces these enzymes and helps to break down food in the digestive system. High levels of amylase and lipase in the blood can indicate inflammation or damage to the pancreas.
In addition to enzyme tests, other laboratory tests that may diagnose pancreatic dysfunction include blood glucose tests, which can detect diabetes, and tests for pancreatic hormones, such as insulin and glucagon. These tests can help identify problems with the pancreas’ production or regulation of these hormones.
It is important to note that laboratory tests alone cannot diagnose iron overload or pancreatic dysfunction. Diagnostic tests, such as imaging studies or biopsies, may also be necessary to confirm a diagnosis. Therefore, it is important to consult with a healthcare provider if you are experiencing symptoms that may indicate a problem with your iron levels or pancreatic Function.
Imaging techniques for assessing iron deposition in organs
Iron deposition in organs can be assessed using various imaging techniques. Some commonly used techniques include:
- Magnetic resonance imaging (MRI): MRI can detect iron deposition in organs such as the liver, spleen, and heart. MRI uses a magnetic field and radio waves to create detailed images of the internal organs.
- Transcranial ultrasound: This technique uses high-frequency sound waves to detect iron deposits in the brain. It is commonly used to screen for iron deposition in patients with hereditary hemochromatosis.
- Computed tomography (CT): CT scans can detect iron deposition in the liver and other organs. CT uses X-rays to create detailed cross-sectional images of the internal organs.
- Dual-energy X-ray absorptiometry (DXA): This technique primarily measures bone density but can also detect iron deposition in the liver.
- Positron emission tomography (PET): PET scans can detect iron deposition in the brain and other organs. PET uses a small amount of radioactive material to create images of the internal organs.
It’s important to note that different imaging techniques have advantages and limitations, and the choice of imaging modality may depend on the specific clinical question and the patient’s clinical presentation.
Importance of genetic testing in identifying hereditary hemochromatosis
Hereditary hemochromatosis (HH) is a genetic disorder characterized by excessive iron absorption and accumulation in various organs such as the liver, pancreas, and heart. Excessive iron deposition can lead to tissue damage and organ failure if left untreated. Genetic testing is crucial in identifying individuals with HH and their family members who may be at risk of developing the disorder.
Several genes are associated with HH, but the most common is the HFE gene. Mutations in the HFE gene are responsible for up to 90% of cases of HH. Genetic testing for HH involves analyzing the HFE gene for mutations associated with the disorder.
There are several reasons why genetic testing is important in identifying hereditary hemochromatosis:
- Early detection: Genetic testing can identify individuals at risk of developing HH before they show any symptoms. This allows for early intervention and treatment, preventing or delaying the onset of complications.
- Accurate diagnosis: Genetic testing is the most reliable method for diagnosing HH. It can distinguish between HH and other iron overload disorders with similar symptoms.
- Family screening: HH is an autosomal recessive disorder, meaning an individual must inherit two copies of the mutated gene (one from each parent) to develop the disorder. Genetic testing can identify family members who are carriers of the mutated gene and at risk of passing it on to their children.
- Tailored treatment: The severity of HH can vary depending on the specific gene mutation and other factors. Genetic testing can help healthcare providers tailor treatment to the individual’s needs and genetic makeup.
In summary, genetic testing is important for identifying hereditary hemochromatosis and managing the disorder. It can facilitate early detection, accurate diagnosis, family screening, and tailored treatment.
Management of Bronze Diabetes
Bronze diabetes, also known as hemochromatosis-related diabetes, is a rare complication of hereditary hemochromatosis (HH), a genetic disorder that leads to iron overload in the body. In bronze diabetes, iron deposits in the pancreas damage the beta cells that produce insulin, leading to diabetes mellitus.
Management of bronze diabetes involves both treating the underlying HH and managing diabetes.
- Treatment of HH: The primary treatment for bronze diabetes is to manage the underlying hemochromatosis. This may involve regular phlebotomy, which removes blood from the body to reduce iron levels. Chelation therapy, which involves taking medications that bind to excess iron and remove it from the body, may also be used in some cases.
- Diabetes management: Diabetes in bronze diabetes is typically managed using the same methods as in other diabetes mellitus. This may include:
- Dietary modifications: A balanced diet rich in fibre, low in fat and refined sugars, and high in complex carbohydrates can help manage blood sugar levels.
- Exercise: Regular physical activity can help improve insulin sensitivity and manage blood sugar levels.
- Medications: Medications such as insulin or oral hypoglycemic agents may be prescribed to help manage blood sugar levels.
- Monitoring: Regular blood glucose levels, iron levels, and organ function monitoring are important in managing bronze diabetes. This can help detect any changes or complications early and allow for prompt intervention.
- Lifestyle modifications: Lifestyle modifications, such as quitting smoking, limiting alcohol intake, and maintaining a healthy weight, can also help manage bronze diabetes and reduce the risk of complications.
It’s important to work closely with a healthcare provider knowledgeable about hemochromatosis and diabetes to develop a personalized treatment plan for bronze diabetes.
A multidisciplinary approach to managing Bronze diabetes
Managing bronze diabetes, a rare complication of hereditary hemochromatosis that leads to diabetes mellitus, requires a multidisciplinary approach that involves various healthcare providers working together to provide comprehensive care. A multidisciplinary team may include the following healthcare providers:
- Primary care physician: The primary care physician is typically the first point of contact for patients with bronze diabetes. They can help manage blood sugar levels, monitor for complications, and refer the patient to other specialists.
- Endocrinologist: An endocrinologist is a specialist who focuses on diagnosing and managing hormone-related disorders, including diabetes. They can help manage insulin therapy, prescribe medications, and monitor for complications related to diabetes.
- Haematologist: A haematologist is a specialist who focuses on blood disorders, including hemochromatosis. They can help manage the underlying hemochromatosis through phlebotomy or chelation therapy and monitor iron levels.
- Gastroenterologist: A gastroenterologist is a specialist who focuses on digestive disorders. In some cases, patients with hemochromatosis may develop liver damage or cirrhosis, and a gastroenterologist can help manage these complications.
- Dietitian: A dietitian can help develop a nutrition plan tailored to the patient’s needs and helps manage blood sugar levels. They can also guide maintaining a healthy weight and limiting alcohol intake.
- Diabetes educator: A diabetes educator can provide education and support to patients with diabetes, including how to manage blood sugar levels, how to administer insulin or other medications, and how to monitor for complications.
- Mental health provider: Diabetes and hemochromatosis can significantly impact a patient’s mental health, and a mental health provider can provide support and counselling to help manage the emotional impact of these conditions.
In summary, managing bronze diabetes requires a multidisciplinary approach that involves various healthcare providers working together to provide comprehensive care. This approach ensures that the patient’s medical and emotional needs are met and receives the best possible care.
Lifestyle modifications, including dietary adjustments and exercise
Lifestyle modifications, including dietary adjustments and exercise, are essential to managing bronze diabetes, a hereditary hemochromatosis complication leading to diabetes mellitus. The following are some lifestyle modifications that can help manage blood sugar levels and reduce the risk of complications:
- Dietary adjustments: A balanced diet rich in fibre, low in fat and refined sugars, and high in complex carbohydrates can help manage blood sugar levels. Patients with bronze diabetes should aim to consume a diet low in iron, as iron overload is a primary cause of the condition. Some dietary adjustments that can help manage bronze diabetes include:
- Limiting intake of red meat, which is high in iron.
- Avoiding iron-fortified foods and supplements.
- Eating more fruits, vegetables, and whole grains.
- Avoiding sugary drinks and foods.
- Exercise: Regular physical activity can help improve insulin sensitivity and manage blood sugar levels. Patients with bronze diabetes should aim to exercise for at least 30 minutes per day, most days of the week. Exercise can take many forms, such as brisk walking, cycling, swimming, or resistance training.
- Smoking cessation: Smoking can increase the risk of complications in patients with bronze diabetes, such as heart disease and nerve damage. Quitting smoking can help reduce the risk of these complications.
- Limiting alcohol intake: Drinking alcohol in excess can increase the risk of liver damage in patients with hemochromatosis. Patients with bronze diabetes should aim to limit their alcohol intake or avoid it altogether.
- Maintaining a healthy weight: Maintaining a healthy weight through diet and exercise can help manage blood sugar levels and reduce the risk of complications. Patients with bronze diabetes should work with their healthcare providers to develop a personalized weight management plan.
In summary, lifestyle modifications, including dietary adjustments and exercise, are important in managing bronze diabetes. Patients with bronze diabetes should work closely with their healthcare providers to develop a personalized lifestyle modification plan that meets their needs and helps manage their blood sugar levels.
Monitoring iron levels and therapeutic phlebotomy as a treatment strategy
Monitoring iron levels and therapeutic phlebotomy are important aspects of managing bronze diabetes, a hereditary hemochromatosis complication leading to diabetes mellitus.
- Monitoring iron levels: Regular monitoring of iron levels is important in managing bronze diabetes. This can help determine if the underlying hemochromatosis is well-controlled and if phlebotomy or chelation therapy is necessary. Iron levels can be monitored through blood tests such as serum ferritin, serum iron, and transferrin saturation.
- Therapeutic phlebotomy: Therapeutic phlebotomy removes blood from the body to reduce iron levels. It is a primary treatment for hemochromatosis and is also used in managing bronze diabetes. The frequency of phlebotomy varies depending on the patient’s iron levels and the severity of their hemochromatosis. Patients with bronze diabetes require more frequent phlebotomy than those with hemochromatosis alone. Phlebotomy aims to maintain iron levels within a normal range and prevent complications related to iron overload.
The following are some key considerations when using therapeutic phlebotomy as a treatment strategy for bronze diabetes:
- Phlebotomy should be performed by a trained healthcare provider and by established protocols.
- Patients should be monitored closely during and after phlebotomy to ensure they do not experience any adverse effects, such as low blood pressure or fainting.
- Patients should be advised to drink plenty of fluids and eat a balanced meal after phlebotomy to help replace the lost blood volume.
- Phlebotomy may be contraindicated in patients who are anaemic, have heart disease, or have other medical conditions that make blood removal unsafe.
In summary, monitoring iron levels and therapeutic phlebotomy are important aspects of managing bronze diabetes. Regular monitoring of iron levels can help determine if phlebotomy or other interventions are necessary, while therapeutic phlebotomy can help reduce iron levels and prevent complications related to iron overload. It’s important to work closely with a healthcare provider knowledgeable about hemochromatosis and bronze diabetes to develop a personalized treatment plan.
Pharmacological interventions for glycemic control
Pharmacological interventions for glycemic control are an important component of managing bronze diabetes, a complication of hereditary hemochromatosis that leads to diabetes mellitus. The following are some common medications used to manage blood sugar levels in patients with bronze diabetes:
- Insulin: Insulin is a hormone the pancreas produces that helps regulate blood sugar levels. In patients with bronze diabetes, insulin therapy may be necessary to manage their diabetes. Insulin can be administered by injection or through an insulin pump.
- Metformin: Metformin is an oral medication that helps lower blood sugar levels by reducing the amount of glucose produced by the liver and improving insulin sensitivity. It is commonly used as a first-line medication in patients with type 2 diabetes, including those with bronze diabetes.
- Sulfonylureas: Sulfonylureas are oral medications that stimulate the pancreas to produce more insulin. They can help lower blood sugar levels in patients with bronze diabetes but may cause hypoglycemia (low blood sugar) and weight gain.
- Dipeptidyl peptidase-4 (DPP-4) inhibitors: DPP-4 inhibitors are oral medications that help lower blood sugar levels by increasing certain hormones that stimulate insulin production. They are typically used as a second-line medication in patients with type 2 diabetes, including those with bronze diabetes.
- Glucagon-like peptide-1 (GLP-1) receptor agonists: GLP-1 receptor agonists are injectable medications that help lower blood sugar levels by increasing insulin production and reducing the amount of glucose produced by the liver. They are typically used as a second-line medication in patients with type 2 diabetes, including those with bronze diabetes.
The choice of medication for glycemic control in patients with bronze diabetes may depend on the patient’s needs and medical history. It’s important to work closely with a healthcare provider knowledgeable about hemochromatosis and diabetes to develop a personalized treatment plan.
Management of associated complications and comorbidities
Bronze diabetes, a hereditary hemochromatosis complication leading to diabetes mellitus, can lead to various complications and comorbidities that require careful management. The following are some common complications and comorbidities associated with bronze diabetes and their management:
- Liver disease: Patients with bronze diabetes and hemochromatosis may be at risk of developing liver diseases, such as cirrhosis or hepatocellular carcinoma. Management may involve regular monitoring of liver function tests and imaging studies and treatment with medications or surgery as necessary.
- Heart disease: Diabetes and hemochromatosis can both increase the risk of heart disease. Management may involve lifestyle modifications, such as quitting smoking, limiting alcohol intake, and maintaining a healthy weight, as well as medications to manage blood pressure, cholesterol levels, and other risk factors.
- Peripheral neuropathy: Diabetes can lead to peripheral neuropathy, which affects the nerves in the hands and feet and can cause numbness, tingling, and pain. Management may involve medications to manage pain and regular foot exams to monitor for complications such as ulcers or infections.
- Retinopathy: Diabetes can lead to retinopathy, a condition that affects the blood vessels in the eyes and can lead to vision loss. Management may involve regular eye exams and treatment with medications or surgery as necessary.
- Kidney disease: Diabetes and hemochromatosis can increase the risk of kidney disease. Management may involve regularly monitoring kidney function tests and urine tests and treatment with medications or dialysis as necessary.
It’s important to work closely with a healthcare provider knowledgeable about hemochromatosis and diabetes to manage any associated complications and comorbidities. Regular monitoring, early detection, and prompt intervention can help prevent or delay the onset of complications and improve overall health outcomes.
Prognosis and Complications
Bronze diabetes, a hereditary hemochromatosis complication leading to diabetes mellitus, can lead to various complications and impact the patient’s prognosis. The following are some common complications and potential impacts on prognosis associated with bronze diabetes:
- Diabetes complications: Diabetes can lead to various complications, including cardiovascular disease, nerve damage, kidney disease, and vision loss. These complications can impact the patient’s quality of life and overall health outcomes.
- Liver disease: Hemochromatosis and bronze diabetes can lead to liver diseases, such as cirrhosis or hepatocellular carcinoma. These conditions can significantly impact the patient’s prognosis and may require ongoing management or treatment.
- Arthropathy: Hemochromatosis and bronze diabetes can lead to arthropathy, which affects the joints and can cause pain, swelling, and stiffness. This can impact the patient’s mobility and quality of life.
- Increased risk of infection: Patients with hemochromatosis and bronze diabetes may be at an increased risk of infection, particularly with organisms that require iron for growth, such as Yersinia enterocolitica. This can impact the patient’s overall health outcomes and may require prompt intervention.
- Increased risk of cancer: Hemochromatosis and bronze diabetes are associated with an increased risk of certain types of cancer, such as hepatocellular carcinoma. Regular monitoring and prompt intervention may be necessary to manage this risk.
It’s important to work closely with a healthcare provider knowledgeable about hemochromatosis and diabetes to manage any associated complications and comorbidities. Regular monitoring, early detection, and prompt intervention can help prevent or delay the onset of complications and improve overall health outcomes. With appropriate management and treatment, many patients with bronze diabetes can lead a full and productive life.
Long-term Outcomes and Prognosis of bronze diabetes
Bronze diabetes, a hereditary hemochromatosis complication leading to diabetes mellitus, can have significant long-term outcomes and prognosis. The following are some potential impacts on long-term outcomes and prognosis associated with bronze diabetes:
- Complications of diabetes: Diabetes can lead to various complications over time, including cardiovascular disease, nerve damage, kidney disease, and vision loss. These complications can impact the patient’s quality of life and overall health outcomes.
- Liver disease: Hemochromatosis and bronze diabetes can lead to liver diseases, such as cirrhosis or hepatocellular carcinoma. These conditions can significantly impact the patient’s long-term outcomes and prognosis and may require ongoing management or treatment.
- Arthropathy: Hemochromatosis and bronze diabetes can lead to arthropathy, which affects the joints and can cause pain, swelling, and stiffness. This can impact the patient’s mobility and quality of life.
- Increased risk of infection: Patients with hemochromatosis and bronze diabetes may be at an increased risk of infection, particularly with organisms that require iron for growth, such as Yersinia enterocolitica. This can impact the patient’s overall health outcomes and may require prompt intervention.
- Increased risk of cancer: Hemochromatosis and bronze diabetes are associated with an increased risk of certain types of cancer, such as hepatocellular carcinoma. Regular monitoring and prompt intervention may be necessary to manage this risk.
- Prognosis: The long-term prognosis for patients with bronze diabetes depends on various factors, including the severity of their hemochromatosis and diabetes, complications or comorbidities, and their response to treatment. With appropriate management and treatment, many patients with bronze diabetes can lead a full and productive life. However, the condition can lead to significant morbidity and mortality if left untreated.
It’s important to work closely with a healthcare provider knowledgeable about hemochromatosis and diabetes to manage any associated complications and comorbidities. Regular monitoring, early detection, and prompt intervention can help prevent or delay the onset of complications and improve overall health outcomes.
Risks and complications associated with iron overload and diabetes
Iron overload and diabetes are two conditions that can have significant risks and complications when they occur together, as in the case of bronze diabetes, a hereditary hemochromatosis complication leading to diabetes mellitus. The following are some common risks and complications associated with iron overload and diabetes:
- Cardiovascular disease: Iron overload and diabetes are associated with an increased risk of cardiovascular diseases, such as heart attack and stroke. This can be due to various factors, including inflammation, oxidative stress, and insulin resistance.
- Liver disease: Iron overload and diabetes can lead to liver diseases like cirrhosis or hepatocellular carcinoma. These conditions can significantly impact the patient’s health outcomes and may require ongoing management or treatment.
- Arthropathy: Iron overload can lead to arthropathy, which affects the joints and can cause pain, swelling, and stiffness. This can be particularly problematic in patients with diabetes, as it can impact their mobility and quality of life.
- Increased risk of infection: Patients with iron overload and diabetes may be at an increased risk of infection, particularly with organisms that require iron for growth, such as Yersinia enterocolitica. This can impact the patient’s overall health outcomes and may require prompt intervention.
- Increased risk of cancer: Iron overload and diabetes are associated with an increased risk of certain types of cancer, such as hepatocellular carcinoma. Regular monitoring and prompt intervention may be necessary to manage this risk.
- Retinopathy: Diabetes can lead to retinopathy, a condition that affects the blood vessels in the eyes and can lead to vision loss. Iron overload may exacerbate this condition by increasing oxidative stress and eye inflammation.
It’s important to work closely with a healthcare provider knowledgeable about hemochromatosis and diabetes to manage any associated risks and complications. Regular monitoring, early detection, and prompt intervention can help prevent or delay the onset of complications and improve overall health outcomes.
Impact of early diagnosis and Intervention on disease progression
Early diagnosis and intervention can significantly impact the disease progression of bronze diabetes, a complication of hereditary hemochromatosis that leads to diabetes mellitus. The following are some potential benefits of early diagnosis and intervention:
- Prevention of complications: Early diagnosis and intervention can help prevent or delay the onset of complications associated with bronze diabetes, such as cardiovascular disease, nerve damage, kidney disease, and vision loss. By managing blood sugar levels and reducing iron overload, patients with bronze diabetes can reduce their risk of developing these complications.
- Improved quality of life: Managing the symptoms and complications of bronze diabetes can significantly impact the patient’s quality of life. Early diagnosis and intervention can help patients maintain their independence, mobility, and overall health, improving their quality of life.
- Improved prognosis: Early diagnosis and intervention can help improve the long-term prognosis for patients with bronze diabetes. By managing their blood sugar levels and iron overload, patients can reduce their risk of developing serious complications and improve their overall health outcomes.
- Preventing transmission to family members: Early diagnosis and intervention can also prevent the transmission of hemochromatosis and bronze diabetes to family members. Identifying affected family members early can help them receive appropriate treatment and prevent the development of complications.
- More effective treatment: Early diagnosis and intervention can help patients receive more effective treatment for their condition. By identifying and managing their condition early, patients with bronze diabetes can avoid the need for more invasive or aggressive treatments later on.
In summary, early diagnosis and intervention can significantly impact the disease progression of bronze diabetes. By managing blood sugar levels and reducing iron overload, patients can prevent or delay the onset of complications, improve their quality of life, and improve their long-term prognosis. It’s important to work closely with a healthcare provider knowledgeable about hemochromatosis and diabetes to receive early diagnosis and appropriate treatment.
Strategies for preventing and managing complications
Preventing and managing complications is an important aspect of managing bronze diabetes, a hereditary hemochromatosis complication leading to diabetes mellitus. The following are some strategies for preventing and managing complications associated with bronze diabetes:
- Regular monitoring: Regular monitoring of blood sugar levels, iron levels, liver function tests, and other relevant tests can help identify any potential complications early on. This can help prevent or delay the onset of complications and improve overall health outcomes.
- Lifestyle modifications: Lifestyle modifications, such as maintaining a healthy weight, eating a balanced diet, exercising regularly, quitting smoking, and limiting alcohol intake, can help reduce the risk of complications associated with diabetes and hemochromatosis.
- Medications: Medications, such as insulin, metformin, and other blood sugar-lowering agents, can help manage blood sugar levels and prevent or delay the onset of complications. Medications to manage iron overloads, such as therapeutic phlebotomy or chelation therapy, may also be necessary to prevent or manage complications associated with hemochromatosis.
- Management of comorbidities: Patients with bronze diabetes may have other comorbidities, such as heart or kidney disease, requiring ongoing management. It’s important to work closely with a healthcare provider knowledgeable about hemochromatosis and diabetes to manage any associated complications and comorbidities.
- Regular screenings: Regular screenings, such as eye exams, foot exams, and kidney function tests, can help identify potential complications early on. This can help prevent or delay the onset of complications and improve overall health outcomes.
Patient Education and Support
Patient education and support are critical components of managing bronze diabetes, a hereditary hemochromatosis complication leading to diabetes mellitus. The following are some ways healthcare providers can provide education and support to patients with bronze diabetes:
- Explanation of the condition: Healthcare providers should explain the condition to patients, including how it develops, the symptoms, and the potential complications.
- Lifestyle modifications: Healthcare providers should provide information on lifestyle modifications that can help manage the condition, such as a healthy diet, exercise, and smoking cessation.
- Medication management: Healthcare providers should provide education on the medications used to manage bronze diabetes, including their indications, dosing, and potential side effects.
- Monitoring: Healthcare providers should explain the importance of regularly monitoring blood sugar levels, iron levels, liver function tests, and other relevant tests. They should also provide guidance on how to monitor these parameters at home and what to do if there are any concerns.
- Management of comorbidities: Healthcare providers should provide education on the management of any comorbidities associated with bronze diabetes, such as heart disease or kidney disease.
- Support groups: Healthcare providers may recommend support groups for patients with bronze diabetes, which can provide emotional support and information on managing the condition.
- Referral to specialists: Healthcare providers may refer patients to specialists, such as endocrinologists, haematologists, or dieticians, for additional support and guidance.
Importance of patient education in bronze diabetes management
Patient education is essential in managing bronze diabetes, a hereditary hemochromatosis complication leading to diabetes mellitus. The following are some of the reasons why patient education is important in bronze diabetes management:
- Understanding the condition: Patient education helps patients understand the condition, including how it develops, the symptoms, and the potential complications. This can help patients become more engaged in their care and make informed decisions about their treatment.
- Lifestyle modifications: Patient education can help patients understand the importance of lifestyle modifications, such as a healthy diet, exercise, and smoking cessation, in managing bronze diabetes. Patients who understand the importance of these modifications are more likely to adhere to them, which can improve their overall health outcomes.
- Medication management: Patient education can help patients understand the medications used to manage bronze diabetes, including their indications, dosing, and potential side effects. Patients who understand how their medications work are more likely to take them as prescribed, which can improve their blood sugar control and prevent complications.
- Monitoring: Patient education can help patients understand the importance of regular monitoring of blood sugar levels, iron levels, liver function tests, and other relevant tests. Patients who understand how to monitor these parameters at home and what to do if there are any concerns are more likely to engage in self-management and prevent complications.
- Management of comorbidities: Patient education can help patients understand the importance of managing any comorbidities associated with bronze diabetes, such as heart disease or kidney disease. Patients who understand the importance of managing these comorbidities are more likely to adhere to their treatment plans, which can improve their overall health outcomes.
In summary, patient education is a critical component of bronze diabetes management. Patient education helps patients understand the condition, lifestyle modifications, medication management, monitoring, and management of comorbidities. By providing education, healthcare providers can help patients become more engaged in their care and improve their overall health outcomes.
Understanding the impact of lifestyle modifications and treatment adherence
Lifestyle modifications and treatment adherence can significantly impact the management of bronze diabetes, a complication of hereditary hemochromatosis that leads to diabetes mellitus. The following are some of how lifestyle modifications and treatment adherence can impact the management of bronze diabetes:
- Blood sugar control: Lifestyle modifications, such as a healthy diet, exercise, and weight management, can help improve blood sugar control in patients with bronze diabetes. Adherence to medication regimens, including insulin and other blood sugar-lowering agents, can also help improve blood sugar control. Improved blood sugar control can help prevent or delay the onset of complications associated with diabetes.
- Iron overload management: Lifestyle modifications, such as limiting iron-rich foods and avoiding iron supplements, can help reduce iron overload in patients with hemochromatosis. Adherence to therapeutic phlebotomy or chelation therapy regimens can also help reduce iron overload. Improved management of iron overload can help prevent or delay the onset of complications associated with hemochromatosis.
- Management of comorbidities: Lifestyle modifications, such as a healthy diet and exercise, can help manage comorbidities associated with bronze diabetes, such as heart and kidney disease. Adherence to medication regimens for these comorbidities can also help improve management.
- Quality of life: Lifestyle modifications and treatment adherence can improve the patient’s quality of life by managing symptoms and reducing the risk of complications associated with bronze diabetes. Patients who adhere to their treatment plans are more likely to experience improved overall health outcomes and a higher quality of life.
Resources and support systems for individuals with bronze diabetes and hemochromatosis
Several resources and support systems are available for individuals with bronze diabetes and hemochromatosis, which can help them manage their condition and improve their overall health outcomes. Some of the resources and support systems include:
- Healthcare providers: Healthcare providers, including primary care physicians, endocrinologists, and haematologists, can provide medical care and management for individuals with bronze diabetes and hemochromatosis.
- Patient support groups: Patient support groups, such as the Iron Disorders Institute or the Hemochromatosis Foundation, can provide emotional support and information on managing the condition.
- Nutritionists: Nutritionists can guide dietary modifications to reduce iron intake and manage diabetes.
- Social workers: Social workers can assist with navigating the healthcare system and accessing resources such as financial assistance programs and transportation services.
- Genetic counselling: Genetic counselling can provide information and support for individuals and their families at risk of hereditary hemochromatosis.
- Online resources: There are several online resources available, such as the National Hemochromatosis Registry, that provide information on the condition, management strategies, and available resources.
Psychological Aspects and coping strategies for Patients and their families
Bronze diabetes and hemochromatosis can significantly impact the psychological well-being of patients and their families. Coping strategies and psychological support can help individuals and their families manage these conditions’ emotional and psychological aspects. The following are some coping strategies and psychological support options for patients and their families:
- Education: Education about the condition can help patients and their families understand the disease process, treatment options, and potential complications. This can help reduce fear and anxiety and increase feelings of control and empowerment.
- Support groups: Support groups like the Iron Disorders Institute or the Hemochromatosis Foundation can provide emotional support and a sense of community for patients and their families. Support groups can provide an opportunity to connect with others who are going through similar experiences and share coping strategies.
- Counselling or therapy: Counseling or therapy can help individuals and their families cope with the emotional and psychological aspects of the condition, such as depression, anxiety, and stress. Therapy can provide a safe and supportive environment to express feelings and develop coping skills.
- Mind-body techniques: Mind-body techniques, such as meditation, yoga, and tai chi, can help reduce stress and improve overall well-being.
- Healthy lifestyle choices: Healthy lifestyle choices, such as regular exercise, a balanced diet, and sufficient sleep, can help reduce stress and improve overall well-being.
- Open communication: Open communication between patients and their families can help reduce anxiety and increase feelings of support and understanding. Family members can be important in providing emotional support and assisting with daily management tasks.
Research and Future Directions
Research on bronze diabetes and hemochromatosis is ongoing to improve these conditions’ diagnosis, treatment, and management. Some of the areas of research and future directions include:
- Genetics: Further research on the genetics of hemochromatosis and bronze diabetes can help identify individuals who are at risk of developing these conditions and develop targeted treatment strategies.
- Biomarkers: Research on biomarkers for iron overload and diabetes can help improve the early detection and diagnosis of bronze diabetes.
- Treatment strategies: Research on novel treatment strategies, including new medications and therapies, can improve the management of bronze diabetes and hemochromatosis and prevent complications.
- Prevention: Research on prevention strategies, including public health education and genetic screening programs, can help prevent the development of bronze diabetes and hemochromatosis in at-risk individuals.
- Comorbidities: Research on managing comorbidities associated with bronze diabetes and hemochromatosis, such as heart and kidney disease, can improve overall patient health outcomes.
- Patient-centred care: Research on patient-centred care and patient outcomes can help improve the quality of care and overall well-being of patients with bronze diabetes and hemochromatosis.
In summary, ongoing research on bronze diabetes and hemochromatosis is focused on improving the early detection, diagnosis, and management of these conditions. Genetics, biomarkers, treatment strategies, prevention, comorbidities, and patient-centered care are all areas of research and future directions that have the potential to improve the quality of care and outcomes for patients with these conditions.
Overview of current research in the field of hemochromatosis and bronze diabetes
There is ongoing research in hemochromatosis and bronze diabetes, focusing on improving these conditions’ diagnosis, treatment, and management. Some current research areas in this field include:
- Genetics: Studies are being conducted to understand better the genetic basis of hemochromatosis and bronze diabetes, including identifying new genetic markers and studying gene expression patterns.
- Biomarkers: Research is being done to identify biomarkers for iron overload and diabetes, which can help improve the early detection and diagnosis of bronze diabetes.
- Treatment strategies: Research is being conducted on new medications and therapies for managing hemochromatosis and bronze diabetes, including studies using novel chelators, iron-targeted drugs, and gene therapy.
- Prevention: Research is being done to evaluate the effectiveness of screening and prevention strategies for hemochromatosis, such as identifying at-risk populations and early intervention.
- Comorbidities: Studies are being conducted to better understand the relationship between hemochromatosis, diabetes, and other comorbidities, such as liver disease and heart disease, and to develop more effective treatment approaches.
- Patient-centred care: Research is being conducted to improve the quality of care and outcomes for patients with hemochromatosis and bronze diabetes, including studies on patient education and engagement, shared decision-making, and telemedicine.
Potential areas of further investigation and advancements
There are several potential areas of further investigation and advancements in the field of hemochromatosis and bronze diabetes. Some of these areas include:
- Precision medicine: The use of precision medicine, which involves the use of individualized genetic and clinical information to guide treatment decisions, could help improve the management of hemochromatosis and bronze diabetes.
- Gene editing: Gene editing techniques, such as CRISPR/Cas9, could correct genetic mutations that cause hemochromatosis and prevent the development of bronze diabetes.
- Stem cell therapy: Stem cell therapy could regenerate damaged tissues in patients with hemochromatosis and bronze diabetes.
- Artificial pancreas: The development of an artificial pancreas, which would mimic the Function of the pancreas in regulating blood sugar levels, could improve the management of diabetes in patients with hemochromatosis.
- Health informatics: The use of health informatics, which involves the analysis of large amounts of health data, could help identify new risk factors for hemochromatosis and improve the early detection and diagnosis of the condition.
- Patient-reported outcomes: The use of patient-reported outcomes, which involve patients reporting on their health outcomes and experiences, could help improve patient-centred care and treatment decisions.
Importance of raising awareness and improving diagnostic capabilities
Raising awareness and improving diagnostic capabilities are essential in managing hemochromatosis and bronze diabetes. The following are some reasons why raising awareness and improving diagnostic capabilities are important:
- Early detection: Raising awareness of hemochromatosis and bronze diabetes can help individuals identify the signs and symptoms of these conditions and seek medical attention early, improving outcomes.
- Timely treatment: Early detection and diagnosis of hemochromatosis and bronze diabetes can lead to timely treatment and management, reducing the risk of complications.
- Population screening: Raising awareness of hemochromatosis and bronze diabetes can also lead to increased population screening, which can identify individuals at risk of developing these conditions and prevent complications.
- Family screening: Raising awareness of hemochromatosis and bronze diabetes can also lead to increased family screening, identifying family members at risk of developing these conditions and preventing complications.
- Improved quality of life: Early detection, timely treatment, and management of hemochromatosis and bronze diabetes can lead to improved quality of life for patients, including better blood sugar control, reduced iron overload, and a reduced risk of complications.
- Research: Increased awareness and improved diagnostic capabilities can also lead to increased research on hemochromatosis and bronze diabetes, improving our understanding of these conditions and leading to new treatment approaches.
Collaboration between healthcare professionals, researchers, and advocacy groups
Collaboration between healthcare professionals, researchers, and advocacy groups is essential in improving the diagnosis, treatment, and management of hemochromatosis and bronze diabetes. The following are some reasons why collaboration is important:
- Knowledge sharing: Collaboration can facilitate the sharing of knowledge and expertise among healthcare professionals, researchers, and advocacy groups, which can improve the understanding of these conditions and lead to new treatment approaches.
- Improved patient care: Collaboration can also lead to improved patient care. Healthcare professionals and advocacy groups work together to develop personalized treatment plans that meet the unique needs of patients with hemochromatosis and bronze diabetes.
- Research: Collaboration between researchers and healthcare professionals can lead to more robust and relevant research on hemochromatosis and bronze diabetes, improving our understanding of these conditions and leading to new treatment approaches.
- Advocacy: Advocacy groups are important in raising awareness of hemochromatosis and bronze diabetes and advocating for increased research funding and improved patient care. Collaboration between healthcare professionals, researchers, and advocacy groups can amplify advocacy efforts and achieve common goals.
- Training and education: Collaboration can also lead to improved training and education for healthcare professionals and patients, improving the quality of care and management of hemochromatosis and bronze diabetes.
Conclusion
Recap of the key features and implications of bronze diabetes
Bronze diabetes is a rare form of diabetes that occurs in individuals with hereditary hemochromatosis, a condition characterized by excessive iron accumulation in the body. Some key features and implications of bronze diabetes include:
- Cause: Bronze diabetes is caused by iron accumulation in the pancreas, which damages the insulin-producing cells and leads to diabetes.
- Symptoms: Bronze diabetes can cause symptoms similar to type 1 and type 2 diabetes, including increased thirst, frequent urination, fatigue, and blurred vision.
- Diagnosis: Diagnosis of bronze diabetes involves testing for both hemochromatosis and diabetes and monitoring iron levels in the body.
- Management: Management of bronze diabetes involves a multidisciplinary approach, including lifestyle modifications, pharmacological interventions, and therapeutic phlebotomy to remove excess iron.
- Complications: Complications of bronze diabetes can include heart disease, liver disease, and kidney disease, as well as complications associated with diabetes.
- Prognosis: Early diagnosis and treatment of bronze diabetes can improve outcomes and prevent complications, but untreated or poorly managed bronze diabetes can lead to significant health problems and reduced life expectancy.
Emphasis on early detection, proper management, and regular monitoring
Early detection, proper management, and regular monitoring are essential in managing bronze diabetes. The following are some reasons why early detection, proper management, and regular monitoring are important:
- Early detection: Early detection of bronze diabetes can lead to timely treatment and management, reducing the risk of complications.
- Proper management: The management of bronze diabetes involves a multidisciplinary approach, including lifestyle modifications, pharmacological interventions, and therapeutic phlebotomy to remove excess iron. Proper management can improve blood sugar control, reduce iron overload, and prevent complications.
- Regular monitoring: Regular monitoring of iron and blood sugar levels is essential in managing bronze diabetes, as it can help healthcare professionals make informed decisions about treatment and management.
- Improved quality of life: Early detection, proper management, and regular monitoring of bronze diabetes can lead to improved quality of life for patients, including better blood sugar control, reduced iron overload, and a reduced risk of complications.
- Prevention of complications: Regular monitoring can help identify complications early, leading to timely intervention and prevention of further complications.
Early detection, proper management, and regular monitoring are important in managing bronze diabetes. Early detection can lead to timely treatment, proper management can reduce the risk of complications, regular monitoring can help healthcare professionals make informed decisions about treatment and management, and all of these can lead to an improved quality of life for patients with this condition. Healthcare providers should emphasize the importance of early detection, proper management, and regular monitoring of their patients with hemochromatosis and raise awareness about the potential complications of untreated or poorly managed bronze diabetes.
Importance of a multidisciplinary approach and individualized care
A multidisciplinary approach and individualized care are essential in managing bronze diabetes. The following are some reasons why a multidisciplinary approach and individualized care are important:
- Comprehensive care: A multidisciplinary approach involves a team of healthcare professionals, including endocrinologists, haematologists, nutritionists, and diabetes educators, working together to develop a comprehensive care plan for patients with bronze diabetes. This can lead to more personalized and effective treatment approaches.
- Tailored care: Individualized care involves tailoring treatment plans to meet each patient’s unique needs. This can involve addressing individual lifestyles, comorbidities, and genetic factors affecting treatment outcomes.
- Improved patient outcomes: A multidisciplinary approach and individualized care can improve patient outcomes, including better blood sugar control, reduced iron overload, and a reduced risk of complications.
- Patient-centred care: A multidisciplinary approach and individualized care also emphasize patient-centred care, which involves engaging patients in their care and empowering them to make informed decisions about their health.
- Better communication: A multidisciplinary approach involves improved communication among healthcare professionals, which can lead to more effective and coordinated care for patients.
A multidisciplinary approach and individualized care are essential in managing bronze diabetes. Comprehensive, tailored, improved patient outcomes, patient-centred care, and better communication are potential benefits of a multidisciplinary approach and individualized care. Healthcare providers should collaborate to develop collaborative partnerships and personalized care plans to improve the lives of those affected by this condition.
Prospects and hope for improved outcomes in individuals with bronze
There is hope for improved outcomes in individuals with bronze diabetes. The following are some potential areas of development that could lead to improved outcomes:
- Improved screening: Improved screening strategies can help identify individuals at risk of developing hemochromatosis and bronze diabetes earlier, allowing for earlier intervention and treatment.
- Precision medicine: Precision medicine approaches, which involve tailoring treatment plans to patients’ unique genetic and clinical profiles, could lead to more personalized and effective treatments for individuals with bronze diabetes.
- Novel therapies: Developing novel therapies, including iron-targeted drugs, chelators, and gene therapy, could lead to new treatment approaches that can better manage iron overload and improve blood sugar control.
- Patient education: Increased patient education and engagement can help patients with bronze diabetes better understand their condition, make informed decisions about their health, and adhere to treatment plans.
- Advocacy and awareness: Increased advocacy and awareness of hemochromatosis and bronze diabetes can help improve public understanding of these conditions and increase funding for research, leading to improved treatment options and outcomes.