Foot Wounds Not Healing: Common Causes
Foot wounds that are not healing correctly can cause concern, particularly for individuals with diabetes. In this article, we will explore the common causes of non-healing foot wounds, the potential complications they can lead to, and various management strategies that can promote wound healing and prevent further complications.
Importance of proper wound healing, particularly in the feet
Proper wound healing is essential to ensure that injuries and wounds are treated effectively and do not lead to complications or long-term health issues. This is particularly important regarding wounds on the feet, as the feet are a critical part of the body that supports our weight and enable us to move around.
Here are some reasons why proper wound healing is so important, especially for wounds on the feet:
- Prevention of infection: Wounds on the feet are particularly susceptible to disease due to the moist and warm environment created by wearing shoes or socks. Proper wound healing can help prevent infection from developing and spreading, leading to serious health issues if left untreated.
- Improved circulation: Wound healing can help improve foot circulation, essential for maintaining healthy tissue and preventing further injury.
- Pain relief: Proper wound healing can help to reduce pain associated with injuries or wounds on the feet. This is particularly important for individuals who suffer from chronic foot pain or conditions such as diabetic neuropathy.
- Prevention of complications: Proper wound healing can help to prevent complications such as foot ulcers, which can be challenging to treat and may require surgery or other invasive procedures.
- Faster recovery: Proper wound healing can speed up recovery and allow individuals to return to daily activities more quickly.
Proper wound healing is crucial for maintaining the health and well-being of the feet. If you have a wound or injury on your feet, it is essential to seek medical attention and follow proper wound care techniques to ensure that it heals properly and does not lead to further complications.
Definition of non-healing foot wound
Non-healing foot wounds, also known as chronic wounds, are wounds on the foot that do not heal properly and remain open for an extended period, often for several weeks or even months. Various factors, such as diabetes, poor circulation, nerve damage, or a compromised immune system, can cause these wounds. Non-healing foot wounds can be particularly concerning, leading to severe complications and even amputation if left untreated.
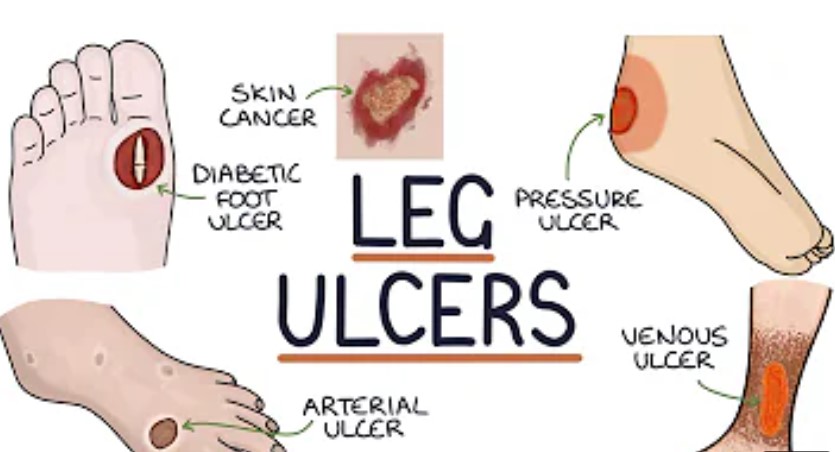
Non-healing foot wounds can be classified into different types based on their cause and location, such as:
- Diabetic foot ulcers are wounds that develop in people with diabetes due to nerve damage, poor circulation, and other factors that can slow the healing process.
- Pressure ulcers are wounds that develop when prolonged pressure is applied to an area of the foot, such as when a person sits or lies down for an extended period.
- Venous stasis ulcers: These are wounds that develop due to poor circulation in the legs, which can lead to fluid accumulation and tissue breakdown.
- Arterial ulcers are wounds that develop due to poor circulation caused by narrowing or blockage of the arteries that supply blood to the feet.
Non-healing foot wounds require prompt medical attention and proper wound care to ensure they heal properly and do not lead to further complications. Treatment may include cleaning and dressing the wound, medication to control infection or inflammation, and therapies to promote healing, such as hyperbaric oxygen therapy or skin grafting.
Overview of the impact of non-healing wounds on overall health
Non-healing wounds, particularly in the feet, can have a significant impact on overall health, both physically and emotionally. Here are some ways in which non-healing damages can affect a person’s health:
- Increased risk of infection: Non-healing wounds are more susceptible to disease, leading to a range of complications, such as cellulitis, osteomyelitis, or sepsis. These infections can be life-threatening, especially in people with weakened immune systems.
- Delayed healing: Non-healing wounds can take weeks, months, or even years, leading to prolonged pain, discomfort, and impaired mobility. This can significantly impact a person’s quality of life and ability to perform daily activities.
- Reduced physical activity: Non-healing wounds can limit a person’s ability to engage in physical activities, such as walking, exercising, or working. This can lead to a sedentary lifestyle, increasing the risk of other health problems like obesity, diabetes, or cardiovascular disease.
- Emotional distress: Non-healing wounds can cause emotional pain, such as anxiety, depression, and social isolation. This is especially true for people with chronic wounds that are difficult to treat and significantly impact their daily lives.
- Increased healthcare costs: Non-healing wounds can be costly, requiring frequent medical visits, wound care supplies, and other interventions. This can place a significant financial burden on patients and their families.
In conclusion, non-healing wounds can profoundly impact overall physical and emotional health. Prompt medical attention, proper wound care, and lifestyle modifications can help to prevent and manage non-healing injuries and their complications.
Common Causes of Non-healing Foot Wounds
Non-healing foot wounds can be caused by various factors, including medical conditions, lifestyle choices, and environmental factors. Here are some of the most common causes of non-healing foot wounds:
- Diabetes: Diabetes is one of the most common causes of non-healing foot wounds. High blood sugar levels can damage nerves and blood vessels in the feet, reducing sensation and blood flow to the affected area. This can result in the development of foot ulcers that are slowly healing and can become infected.
- Peripheral arterial disease (PAD): PAD is a condition that occurs when the blood vessels in the legs and feet become narrowed or blocked. This can lead to poor blood flow to the affected area, reducing the oxygen and nutrients needed for wound healing.
- Venous insufficiency: Venous insufficiency is a condition that occurs when the veins in the legs and feet do not function properly, leading to poor blood flow and the accumulation of fluid. This can result in chronic wounds, such as venous ulcers.
- Trauma: Trauma to the feet, such as cuts, bruises, or burns, can result in non-healing wounds. This is especially true for people with poor circulation or a compromised immune system, as these conditions can slow healing.
- Poor foot care: Poor foot care, such as wearing ill-fitting shoes, not keeping the feet clean and dry, or not trimming toenails properly, can increase the risk of developing non-healing wounds.
- Smoking: Smoking can hurt circulation and immune function, making it harder for wounds to heal correctly.
- Ageing can decrease circulation and immune function, making wound healing difficult.
Identifying the underlying cause of non-healing foot wounds is essential to develop an appropriate treatment plan. Treatment may include wound care, medication, lifestyle modifications, and, in severe cases, surgery.
Diabetic foot ulcers
Diabetic foot ulcers are a common complication of diabetes that can lead to serious health problems if left untreated. They are open sores or wounds that typically develop on the bottom of the foot but can also occur on the top or sides of the foot, toes, or heel.
Diabetic foot ulcers are caused by a combination of factors, including nerve damage (neuropathy), poor circulation, and high blood sugar levels. Neuropathy can cause a loss of sensation in the feet, making it difficult to detect injuries or irritation that can lead to ulcers. Poor circulation can impair the body’s ability to deliver nutrients and oxygen to the affected area, slowing the healing process. High blood sugar levels can also impair immune function and increase the risk of infection.
Symptoms of diabetic foot ulcers include:
- Open sores or wounds that do not heal or show signs of improvement over time
- Drainage or pus from the wound
- A foul odour coming from the wound
- Redness, swelling, or warmth around the affected area
- Pain or discomfort in the affected area
Treatment for diabetic foot ulcers typically involves a combination of wound care, medication, and lifestyle modifications. This may include cleaning and dressing the wound, antibiotics to control infection, and blood sugar control. In severe cases, surgery may be necessary to remove damaged tissue or correct underlying problems such as foot deformities.
Prevention is also an essential aspect of managing diabetic foot ulcers. This includes regular foot exams, proper foot care, wearing appropriate footwear, and controlling blood sugar levels through diet, exercise, and medication.
Peripheral arterial disease (PAD)
Peripheral arterial disease (PAD) is a condition that affects the blood vessels that carry oxygen and nutrients to the limbs, most commonly the legs. It occurs when the blood vessels become narrowed or blocked due to the buildup of plaque, which can lead to reduced blood flow to the affected area.
The most common cause of PAD is atherosclerosis, a condition in which fatty deposits build up on the walls of the arteries. Other risk factors for PAD include smoking, high blood pressure, high cholesterol, diabetes, and a family history of the disease.
Symptoms of PAD include:
- Pain or cramping in the legs, thighs, or buttocks during physical activity, which is relieved with rest (intermittent claudication)
- Numbness or weakness in the legs
- Sores or wounds on the feet or toes that do not heal or heal slowly
- Coldness or discolouration of the affected area
- Weak or absent pulse in the affected limb
If left untreated, PAD can lead to severe complications, such as tissue death (gangrene), infections, and amputation. Therefore, early diagnosis and management are crucial.
Treatment for PAD typically involves lifestyle modifications, medication, and surgery. Lifestyle modifications may include exercise, smoking cessation, and dietary changes. Prescriptions may include blood thinners or medications to control blood pressure or cholesterol levels. Surgery may sometimes be necessary to remove blockages or bypass the affected area.
Prevention is also crucial for people at risk of developing PAD. This includes managing risk factors such as high blood pressure, high cholesterol, and diabetes and adopting healthy lifestyle habits such as regular exercise and avoiding smoking.
Venous insufficiency
Venous insufficiency is a condition that occurs when the veins in the legs do not function properly, leading to poor blood flow and the accumulation of blood in the lower legs. This can result in various symptoms, such as swelling, pain, and the development of varicose veins.
The most common cause of venous insufficiency is damage to the valves in the veins that generally help prevent blood backflow. Various factors, including genetics, obesity, pregnancy, and prolonged sitting or standing, can cause this damage.
Symptoms of venous insufficiency include:
- Swelling in the legs, ankles, or feet
- Aching, throbbing, or cramping in the legs
- Varicose veins
- Skin changes, such as thickening or discolouration
- Open sores or ulcers that do not heal or heal slowly
Treatment for venous insufficiency typically involves a combination of lifestyle modifications and medication. Lifestyle modifications may include exercise, elevation of the legs, and wearing compression stockings. Prescriptions may include drugs that help improve blood flow, reduce swelling, or prevent blood clots.
In some cases, surgery may be necessary to remove varicose veins or repair damaged valves in the veins. This may involve sclerotherapy, laser treatment, or vein stripping.
Prevention is also crucial for people at risk of developing venous insufficiency. This includes maintaining a healthy weight, staying physically active, avoiding prolonged sitting or standing, and wearing compression stockings if a healthcare provider recommends it.
Pressure ulcers
Pressure ulcers, also known as bedsores or pressure sores, are injuries to the skin and underlying tissues caused by prolonged pressure on the skin. They typically occur in people who are immobilized or have limited mobility, such as those who are bedridden or in a wheelchair.
Pressure ulcers can develop quickly, sometimes within hours, and progress rapidly if left untreated. They most commonly occur on bony areas of the body, such as the hips, tailbone, heels, and ankles.
Other factors contributing to the development of pressure ulcers include friction, shear, moisture, poor nutrition, and medical conditions that affect blood flow or sensation.
Symptoms of pressure ulcers may include:
- Redness or discolouration of the affected area
- Swelling or warmth around the affected area
- Pain or tenderness in the affected area
- A blister or open sore on the skin
- Skin that feels different than surrounding areas, such as firmer or softer
Treatment for pressure ulcers typically involves removing the pressure from the affected area and providing wound care. This may include cleaning the wound, applying dressings or ointments, and promoting healing, such as using specialized beds or cushions.
Prevention is also crucial for people at risk of developing pressure ulcers. This includes repositioning the body frequently to relieve pressure, using cushions or pillows to protect bony areas, keeping the skin clean and dry, and maintaining good nutrition and hydration.
If left untreated, pressure ulcers can lead to severe complications such as infections, sepsis, or even death. Therefore, it is essential to seek medical attention if you suspect you have a pressure ulcer or any skin injury that does not heal within a reasonable amount of time.
Infection
The invasion and multiplication of harmful microorganisms such as bacteria, viruses, fungi, or parasites in the body cause infection. Infections can occur anywhere in the body, including in the skin, respiratory tract, urinary tract, and bloodstream.
Common symptoms of infection may include fever, fatigue, pain, redness, swelling, and discharge from the affected area. Depending on the type of infection, other symptoms may include coughing, diarrhoea, vomiting, and difficulty breathing.
Infections can range in severity from mild to life-threatening. Soft disorders may resolve independently or with treatment, while severe conditions can cause serious complications, such as organ failure or sepsis.
Treatment for infection typically involves using antibiotics or antiviral medications, depending on the type of microorganism causing the infection. Other treatments may include pain relief, fluids, and rest. Sometimes, hospitalization may be necessary, mainly if the disease is severe or underlying medical conditions increase the risk of complications.
Prevention is also crucial in reducing the risk of infection. This includes practising good hygiene, such as washing hands frequently, covering the mouth and nose when coughing or sneezing, and avoiding close contact with people who are sick. It also includes maintaining a healthy immune system, such as getting enough sleep, exercising regularly, and eating a balanced diet.
Neuropathy and sensory loss
Neuropathy is a condition in which there is damage to the nerves that carry messages from the brain and spinal cord to the rest of the body. Sensory loss is a common symptom of neuropathy and can occur in different ways, depending on which nerves are affected.
Peripheral neuropathy, which affects the nerves in the arms and legs, is a common form of neuropathy. It can cause a range of symptoms, such as numbness, tingling, and burning sensations in the affected area. Sometimes, people may also experience sharp, shooting pains or cramps. These symptoms can be particularly problematic in the feet, leading to a loss of sensation and an increased risk of injuries or ulcers.
Other forms of neuropathy can affect the nerves that control bodily functions, such as digestion, blood pressure, and heart rate. Symptoms may include constipation, dizziness, and difficulty with bladder control.
Various factors, including diabetes, infections, autoimmune disorders, and exposure to toxins, can cause neuropathy. Treatment may involve addressing the underlying cause of the neuropathy and managing symptoms, such as pain or discomfort, with medications.
Prevention is also crucial for people at risk of developing neuropathy. This includes maintaining reasonable blood sugar control in people with diabetes, avoiding exposure to toxins, and managing underlying medical conditions that can increase the risk of neuropathy.
People with neuropathy and sensory loss must protect themselves from injuries and ulcers. This may include regular foot exams, wearing appropriate footwear, and keeping the feet clean and dry.
Poor circulation
Poor circulation is a condition in which reduced blood flow to specific body parts, such as the legs, feet, hands, or brain. Various factors, including underlying medical conditions, lifestyle choices, and genetic factors, can cause this.
Common causes of poor circulation include:
- Peripheral arterial disease (PAD): PAD is when the blood vessels that carry blood to the legs and feet become narrowed or blocked. This can reduce blood flow and oxygen to the affected area, causing pain, cramping, and numbness.
- Diabetes: Diabetes can damage blood vessels and nerves in the feet and legs, reducing blood flow and sensation. This can increase the risk of injuries and infections.
- Smoking can constrict blood vessels and reduce blood flow, increasing the risk of circulation and other health problems such as heart disease and stroke.
- Obesity: Excess body weight can strain the circulatory system and reduce blood flow to specific body areas.
- Raynaud’s disease: Raynaud’s disease is when the blood vessels in the hands and feet overreact to cold temperatures or stress, causing the blood vessels to narrow and reduce blood flow.
Symptoms of poor circulation may include:
- Numbness or tingling in the affected area
- Coldness or discolouration of the skin
- Pain or cramping in the legs or feet
- Slow-healing wounds or ulcers
- Hair loss or slow nail growth in the affected area
Treatment for poor circulation may include lifestyle modifications such as exercise, weight management, smoking cessation, medication, and surgery. In some cases, interventions such as angioplasty, stenting, or bypass surgery may be necessary to improve blood flow.
Prevention is also crucial for people at risk of developing poor circulation. This includes adopting healthy lifestyle habits such as regular exercise, maintaining a healthy weight, avoiding smoking, and managing underlying medical conditions such as diabetes or high blood pressure.
Understanding the Impact of Diabetes on Wound Healing
Diabetes can significantly impact wound healing, particularly in the feet. High blood sugar levels can damage blood vessels and nerves, reducing blood flow and sensation in the affected area. This can increase the risk of injuries, infections and slow healing.
Here are some ways that diabetes can affect wound healing:
- Reduced blood flow: Diabetes can damage blood vessels and reduce blood flow to the affected area. This can impair the delivery of oxygen and nutrients needed for wound healing.
- Neuropathy: Diabetes can cause nerve damage (neuropathy) in the feet, reducing sensation and making it difficult to detect injuries or irritation that can lead to wounds.
- Increased risk of infection: Diabetes weakens the immune system, making it harder to fight off infections. High blood sugar levels can also provide an ideal environment for bacteria to grow and thrive.
- Impaired healing: Diabetes can impair the body’s ability to form new blood vessels and produce collagen, critical components of the wound healing process.
- Chronic wounds: Due to the abovementioned factors, damage in people with diabetes is more likely to become established or non-healing.
Effective wound care for people with diabetes typically involves a multidisciplinary approach that addresses the underlying causes of the wound and any contributing factors, such as poor circulation or infection. Treatment may include:
- Wound cleaning and debridement to remove dead tissue and bacteria
- Dressings and bandages to protect the wound and promote healing
- Antibiotics or other medications to control infection
- Blood sugar control through diet, exercise, and medication
- Offloading to reduce pressure on the affected area
- Surgery or other interventions in severe cases
Prevention is also vital for people with diabetes to reduce the risk of developing wounds. This includes maintaining reasonable blood sugar control, practising good foot care, wearing appropriate footwear, and avoiding smoking. Regular foot exams by a healthcare provider are also recommended to detect and address any potential issues early on.
How diabetes affects wound healing processes
Diabetes can affect wound-healing processes in several ways. High blood sugar levels can damage blood vessels and nerves, reducing blood flow and sensation in the affected area. This can impair the delivery of oxygen and nutrients needed for wound healing. Here are some ways that diabetes can affect wound recovery:
- Reduced blood flow: Diabetes can damage blood vessels and reduce blood flow to the affected area. This can impair the delivery of oxygen and nutrients needed for wound healing.
- Neuropathy: Diabetes can cause nerve damage (neuropathy) in the feet, reducing sensation and making it difficult to detect injuries or irritation that can lead to wounds.
- Increased risk of infection: Diabetes can weaken the immune system, making it harder to fight off infections. High blood sugar levels can also provide an ideal environment for bacteria to grow and thrive.
- Impaired healing: Diabetes can impair the body’s ability to form new blood vessels and produce collagen, critical components of the wound healing process.
- Chronic wounds: Due to the abovementioned factors, damage in people with diabetes is more likely to become established or non-healing.
In addition to these factors, there are other ways that diabetes can affect wound healing, including:
- Poor inflammatory response: Diabetes can affect the body’s inflammatory response, a critical component of wound healing. This can impair the recruitment of immune cells and growth factors needed for recovery.
- Glycation of proteins: High blood sugar levels can cause proteins in the body to become glycated, impairing their function. This can affect the structure and function of proteins involved in wound healing.
- Impaired cell function: Diabetes can impair the operation of various types of cells involved in wound healing, including fibroblasts, which produce collagen, and endothelial cells, which line blood vessels.
Effective wound care for people with diabetes typically involves a multidisciplinary approach that addresses the underlying causes of the wound and any contributing factors, such as poor circulation or infection. Treatment may include wound cleaning, dressings, antibiotics or other medications, blood sugar control, offloading, and surgery or other interventions in severe cases.
The Role of high blood sugar levels in impairing healing mechanisms
High blood sugar levels can impair healing mechanisms in several ways. When blood sugar levels are consistently high, it can lead to hyperglycemia, damaging blood vessels and nerves throughout the body. Here are some ways that high blood sugar levels can impair healing mechanisms:
- Reduced blood flow: High blood sugar levels cause damage to blood vessels, leading to reduced blood flow to the affected area. This can impair the delivery of oxygen and nutrients needed for wound healing.
- Impaired immune response: High blood sugar levels can weaken the immune system, impairing the body’s ability to fight infections. This can increase the risk of wound infections, damaging the healing process.
- Impaired collagen production: High blood sugar levels can impair the body’s ability to produce collagen, an essential component of wound healing. Collagen provides the structure and framework for new tissue growth and helps to strengthen and heal the wound.
- Glycation of proteins: High blood sugar levels can cause proteins in the body to become glycated, impairing their function. This can affect the structure and function of proteins involved in the wound-healing process.
- Impaired cell function: High blood sugar levels can impair the operation of various types of cells involved in wound healing, including fibroblasts, which produce collagen, and endothelial cells, which line blood vessels.
These factors can impair the body’s ability to heal wounds and make it more difficult to achieve successful healing outcomes. Effective management of blood sugar levels through lifestyle changes, medication, and regular medical care is essential for promoting optimal wound healing in people with diabetes.
Importance of blood glucose control in wound management
Blood glucose control is essential to wound management in people with diabetes. High blood sugar levels can impair the body’s ability to heal wounds, making it more difficult to achieve successful healing outcomes. Here are some reasons why blood glucose control is important in wound management:
- Promotes healing: Tight control of blood sugar levels can improve blood flow and enable the delivery of oxygen and nutrients needed for wound healing. It can also help to reduce inflammation and promote healthy tissue growth.
- Reduces risk of infection: High blood sugar levels can weaken the immune system, making it more difficult to fight off infections. Tight control of blood sugar levels can help reduce the risk of wound infections, impairing healing.
- Prevents complications: Poorly controlled blood sugar levels can lead to various difficulties, including nerve damage, kidney damage, and vision problems. These complications can impair the body’s ability to heal wounds and make it more difficult to achieve successful healing outcomes.
- Improves quality of life: Successful wound healing can enhance the quality of life by reducing pain, discomfort, and disability associated with chronic wounds.
Effective management of blood sugar levels involves a combination of lifestyle changes, medication, and regular medical care. This may include following a healthy diet, exercising regularly, taking medication as prescribed, monitoring blood sugar levels regularly, and working closely with healthcare providers to develop a personalized treatment plan.
It is important to note that blood glucose control alone may not be sufficient for successful wound healing. Effective wound care also involves addressing any underlying medical conditions contributing to the wound, such as poor circulation or infection, and promoting healing, such as using appropriate dressings and managing wound drainage. A multidisciplinary approach that involves a team of healthcare providers is often necessary for effective wound management in people with diabetes.
Complications Associated with Non-healing Foot Wounds
Non-healing foot wounds can lead to complications, particularly in people with diabetes. Here are some of the difficulties that can occur:
- Infection: Non-healing wounds can infect, leading to serious complications, including sepsis and cellulitis. Conditions can also delay the healing process and make it more difficult to achieve successful healing outcomes.
- Amputation: In severe cases, non-healing wounds can lead to tissue death (gangrene), which may require amputation of the affected area to prevent the spread of infection or other complications.
- Disability: Chronic non-healing wounds can lead to disability, impairing mobility and quality of life. This can significantly impact the ability to perform daily activities and lead to a loss of independence.
- Reduced quality of life: Non-healing wounds can cause pain, discomfort, and embarrassment, reducing the quality of life. This can also affect mental health and well-being.
- Increased healthcare costs: Non-healing wounds can require regular medical care, including wound care, medication, and hospitalization, which can increase healthcare costs.
Prevention is important in reducing the risk of complications associated with non-healing foot wounds. This includes regular foot exams, good foot hygiene, appropriate footwear, and managing underlying medical conditions such as diabetes or peripheral arterial disease. Effective wound care involves addressing the underlying causes of the wound and any contributing factors, such as poor circulation or infection, and taking steps to promote healing. A multidisciplinary approach that involves a team of healthcare providers is often necessary for effective wound management in people with non-healing foot wounds.
Cellulitis and soft tissue infections
Cellulitis is a bacterial infection of the skin and soft tissues beneath the skin. It can occur anywhere on the body, but it is common in the legs and feet, particularly in people with diabetes or peripheral arterial disease.
Cellulitis typically presents as redness, warmth, swelling, and pain in the affected area. The infection can spread to the lymph nodes and bloodstream in severe cases, leading to more serious complications.
Soft tissue infections, including cellulitis, can be caused by various bacteria, including Staphylococcus aureus and Streptococcus pyogenes. Risk factors for mild tissue infections include skin damage or breaks, such as cuts, blisters, insect bites, and underlying medical conditions that weaken the immune system or impair blood flow.
Treatment for soft tissue infections typically involves antibiotics to control the disease and wound care to promote healing. In severe cases, hospitalization may be necessary, particularly if the disease spreads or underlying medical conditions increase the risk of complications.
Prevention is also important in reducing the risk of cellulitis and soft tissue infections. This includes maintaining good foot hygiene, avoiding skin damage or breaks, and managing underlying medical conditions such as diabetes or peripheral arterial disease.
If you suspect that you may have a soft tissue infection, it is important to seek medical attention promptly. Early treatment can help prevent disease spread and reduce the risk of complications.
Osteomyelitis (bone infection)
Osteomyelitis is a bacterial infection of the bone that can occur in any part of the body but is most commonly seen in the feet and legs. Osteomyelitis can occur due to an open wound or surgery, but it can also happen when an infection in the bloodstream spreads to the bone.
Symptoms of osteomyelitis can include pain, swelling, redness, and warmth in the affected area. In severe cases, fever, chills, and fatigue may also occur. Osteomyelitis can be difficult to treat and may require long-term antibiotics or surgery.
Risk factors for osteomyelitis include:
- Diabetes: Diabetes can impair circulation and increase the risk of foot ulcers, leading to osteomyelitis.
- Peripheral arterial disease: PAD can impair circulation and increase the risk of foot ulcers, leading to osteomyelitis.
- Open wounds: Open wounds, such as those caused by trauma or surgery, can allow bacteria to enter the bone.
- Intravenous drug use: Intravenous drug use can introduce bacteria into the bloodstream, which can spread to the bone.
- Weakened immune system: A weakened immune system can make it more difficult to fight off infections, increasing the risk of osteomyelitis.
Effective treatment of osteomyelitis typically involves a combination of antibiotics or surgery, depending on the severity of the infection. Prevention is also important in reducing the risk of osteomyelitis. This includes maintaining good foot hygiene, avoiding skin damage or breaks, and managing underlying medical conditions such as diabetes or peripheral arterial disease.
If you suspect that you may have osteomyelitis, it is important to seek medical attention promptly. Early diagnosis and treatment can help to prevent the spread of infection and reduce the risk of complications.
Gangrene and tissue necrosis
Gangrene is characterized by tissue death (necrosis) in a body part, typically due to reduced blood flow. It can occur anywhere in the body but is most commonly seen in the feet and legs, particularly in people with diabetes or peripheral arterial disease.
Gangrene can be classified into two types: dry necrosis and wet gangrene. Dry infection occurs when the affected tissue is dehydrated and shrivelled, while wet gangrene is when the affected tissue becomes swollen and discoloured.
Symptoms of gangrene can include pain, swelling, redness, and foul-smelling discharge in the affected area. In severe cases, the affected tissue may turn black and become hard and cold to the touch.
Gangrene is a serious condition that can lead to tissue loss and amputation if not treated promptly. Treatment for gangrene typically involves addressing the underlying cause, such as poor circulation or infection, and removing the affected tissue. In some cases, surgery may be necessary to remove the affected tissue and prevent the spread of disease.
Prevention is also important in reducing the risk of gangrene. This includes maintaining good foot hygiene, avoiding skin damage or breaks, managing underlying medical conditions such as diabetes or peripheral arterial disease, and avoiding tobacco use.
Tissue necrosis is a broader term that refers to the death of any tissue in the body, not just as a result of reduced blood flow. It can occur due to injury, infection, or other causes. Treatment for tissue necrosis typically involves addressing the underlying cause and promoting tissue healing, which may include wound care, antibiotics, surgery, or other interventions depending on the severity and location of the tissue death.
Amputation risk
Non-healing foot wounds, if left untreated or poorly managed, can lead to serious complications, including tissue necrosis, gangrene, and increased risk of amputation. Amputation is a major concern for people with non-healing foot wounds, particularly those with diabetes or peripheral arterial disease.
People with diabetes are at increased risk of amputation due to the combined effects of neuropathy, peripheral arterial disease, and impaired wound healing. Neuropathy can lead to the loss of sensation in the feet, making it difficult to detect injuries or infections that can lead to non-healing wounds. Peripheral arterial disease can impair circulation, reducing blood flow to the affected area and impairing the delivery of oxygen and nutrients needed for healing. Poorly controlled blood sugar levels can also damage the body’s ability to heal wounds, increasing the risk of non-healing injuries and infection.
Early detection and management of non-healing foot wounds are crucial for preventing complications such as amputation. This involves regular foot exams by a healthcare provider to detect and address any potential issues early on. Effective wound care, which addresses the underlying causes of the wound and any contributing factors, such as poor circulation or infection, is also important for promoting healing and reducing the risk of complications.
In severe cases, amputation may be necessary to prevent the spread of infection or other complications. However, with proper management and prevention, many instances of non-healing foot wounds can be successfully treated, and the risk of amputation can be reduced.
Systemic infections and sepsis
Non-healing foot wounds can lead to systemic infections, including sepsis, a potentially life-threatening condition characterized by an extreme response to an infection.
Sepsis occurs when the body’s immune system overreacts to an infection and triggers a chain reaction that can damage multiple organ systems, leading to organ failure and even death if left untreated.
Non-healing foot wounds, particularly in people with diabetes or peripheral arterial disease, can increase the risk of infection, leading to sepsis if not promptly treated. The bacteria that cause the infection can spread from the wound to the bloodstream and throughout the body, leading to sepsis.
Symptoms of sepsis can include fever, chills, rapid breathing, rapid heart rate, confusion, and low blood pressure. Sepsis is a medical emergency and requires prompt treatment to prevent serious complications.
Effective wound care, the underlying causes of the wound, and managing any contributing factors, such as poor circulation or infection, is essential for reducing the risk of systemic diseases and sepsis.
Prevention is also important in reducing the risk of systemic infections and sepsis. This includes maintaining good foot hygiene, avoiding skin damage or breaks, and managing underlying medical conditions such as diabetes or peripheral arterial disease.
If you suspect that you may have a systemic infection or sepsis, it is important to seek medical attention promptly. Early diagnosis and treatment can help prevent disease spread and reduce the risk of complications, including organ failure and death.
Impact on quality of life
Non-healing foot wounds can significantly impact the quality of life of affected individuals. Chronic wounds can cause pain, discomfort, and embarrassment, reducing mobility and quality of life. People with non-healing foot wounds may experience limitations in daily activities, such as walking, standing, and exercising. They may also experience social isolation and depression, particularly if the injuries limit their ability to participate in social activities or work.
In addition to physical and emotional discomfort, non-healing foot wounds can have financial consequences. The cost of wound care, medication, and hospitalization can be significant, particularly for people who require ongoing or long-term treatment. The cost of prosthetics, rehabilitation, and other medical interventions may also concern people who require amputation.
Effective wound care, the underlying causes of the wound, and managing any contributing factors are essential for promoting healing and improving quality of life. Affected individuals must work closely with healthcare providers to develop a personalized treatment plan considering their unique needs and circumstances.
In addition to medical care, social and emotional support can also be helpful for people with non-healing foot wounds. This may involve connecting with support groups, counselling, or other resources to help manage the emotional impact of chronic wounds.
By working with healthcare providers and utilizing appropriate resources and support, people with non-healing foot wounds can improve their quality of life and manage their condition’s physical, emotional, and financial impacts.
Assessment and Diagnosis of Non-healing Foot Wounds
Assessment and diagnosis of non-healing foot wounds typically involve a thorough medical history and physical examination, including an evaluation of the injury and any underlying medical conditions contributing to the damage.
Here are some of the key steps involved in the assessment and diagnosis of non-healing foot wounds:
- Medical history: A healthcare provider will review the individual’s medical record, including any underlying medical conditions such as diabetes or peripheral arterial disease and any medications or treatments that may affect wound healing.
- Physical examination: A healthcare provider will conduct a physical exam, including an evaluation of the wound, the surrounding skin and tissue, and the foot and ankle. They may also perform tests to evaluate circulation and nerve function in the affected area.
- Wound assessment: A healthcare provider will evaluate the wound, including its size, depth, location, and stage of healing. They may also assess the presence of any infection or inflammation and evaluate any drainage or odour associated with the wound.
- Laboratory tests: A healthcare provider may order laboratory tests to evaluate blood sugar levels, white blood cell count, and other indicators of infection or inflammation.
- Imaging tests: A healthcare provider may order imaging tests such as X-rays, ultrasounds, or MRI scans to evaluate the underlying bone, tissue, and circulation in the affected area.
Effective assessment and diagnosis are essential for developing a personalized treatment plan that addresses the underlying causes of the wound and promotes healing. A multidisciplinary approach involving a team of healthcare providers, including wound care specialists, podiatrists, and vascular surgeons, may be necessary to assess, diagnose, and treat non-healing foot wounds effectively.
Comprehensive physical examination
A comprehensive physical examination is important in assessing and diagnosing non-healing foot wounds. A healthcare provider will thoroughly evaluate the affected foot, ankle, and other parts of the body that may contribute to the injury or affect the healing process.
Here are some of the key components of a comprehensive physical examination:
- Foot inspection: A healthcare provider will inspect the affected foot and ankle, looking for any signs of redness, swelling, warmth, or drainage. They will also evaluate the skin for any discolouration, dryness, or cracking, as well as any calluses or corns contributing to the wound.
- Neurological evaluation: A healthcare provider will evaluate the patient’s neurological function, including testing for sensation, reflexes, and muscle strength. This can help identify any underlying nerve damage or neuropathy affecting the healing process.
- Circulation evaluation: A healthcare provider will evaluate the patient’s circulation, including checking for pulses in the foot and ankle, evaluating capillary refill time, and using other tests to assess blood flow to the affected area. This can help identify any underlying peripheral arterial disease or other circulation problems contributing to the wound.
- Range of motion assessment: A healthcare provider will evaluate the patient’s range of motion in the affected foot and ankle, looking for any limitations or abnormalities affecting mobility or healing.
- Assessment of other medical conditions: A healthcare provider will evaluate any other medical conditions contributing to the wound or affecting the healing process, including diabetes, kidney disease, and cardiovascular disease.
A comprehensive physical examination is essential for developing a personalized treatment plan that addresses the underlying causes of the wound and promotes healing. Affected individuals must work closely with healthcare providers to identify any underlying medical conditions or contributing factors affecting the healing process. They must also develop an individualized care plan that meets their unique needs and circumstances.
Evaluation of wound characteristics (size, depth, presence of infection)
Evaluating wound characteristics is important in assessing and diagnosing non-healing foot wounds. A healthcare provider will thoroughly evaluate the injury, looking for specific traits that can help guide treatment and promote healing.
Here are some of the key wound characteristics that healthcare providers will evaluate:
- Size: A healthcare provider will measure the size of the wound, typically in centimetres, to assess the extent of tissue damage and monitor healing progress over time.
- Depth: A healthcare provider will evaluate the depth of the wound, including any involvement of underlying tissues, such as muscle or bone.
- Presence of infection: A healthcare provider will assess the wound for signs of infection, including redness, warmth, swelling, and discharge. They may also order laboratory tests to evaluate the presence of bacteria in the wound.
- Granulation tissue: A healthcare provider will evaluate the wound for the presence of granulation tissue, which is a sign of healing. Granulation tissue appears as pink or red tissue in the base of the injury and is an important indicator of healing progress.
- Exudate: A healthcare provider will evaluate any drainage or exudate from the wound, looking for signs of infection, such as purulent or malodorous discharge.
Effective evaluation of wound characteristics is essential for developing a personalized treatment plan that addresses the underlying causes of the wound and promotes healing. Healthcare providers may use various wound care techniques, including debridement, dressings, and topical medications, to manage wound characteristics and promote healing. They may also address any underlying medical conditions or contributing factors affecting the healing process, such as poor circulation or infection.
Doppler ultrasound for assessing the vascular status
Doppler ultrasound is a non-invasive imaging test that can assess vascular status in people with non-healing foot wounds. The test uses high-frequency sound waves to evaluate blood flow in the arteries and veins of the affected foot and ankle.
During a Doppler ultrasound exam, a healthcare provider will apply a gel to the skin of the affected foot and use a handheld device called a transducer to capture images of the blood flow in the arteries and veins. The images are displayed on a monitor and can help identify any blockages or narrowing in the blood vessels contributing to the non-healing wound.
Doppler ultrasound can provide important information about the affected foot’s vascular status and help guide treatment decisions. For example, if a blockage or narrowing is identified, a healthcare provider may recommend treatments to improve circulation, such as medication or surgery.
Doppler ultrasound is a safe and non-invasive test that typically does not require any special preparation. Depending on the individual’s specific needs and circumstances, the test may be performed in a healthcare provider’s office or a hospital setting.
Doppler ultrasound is an important tool for assessing vascular status in people with non-healing foot wounds and can help guide treatment decisions to promote healing and prevent complications.
Laboratory tests to identify underlying conditions (e.g., diabetes, infection)
Laboratory tests can be used to identify underlying conditions that may be contributing to non-healing foot wounds. Here are some examples of laboratory tests that may be ordered:
- Blood glucose: A blood glucose test measures the amount of glucose (sugar) in the blood and can help to diagnose diabetes or evaluate blood sugar control in people with diabetes.
- Haemoglobin A1C: The haemoglobin A1C test is a blood test that provides an average of blood glucose levels over the past 2-3 months and is used to monitor blood sugar control in people with diabetes.
- Complete blood count (CBC): A CBC measures various components of the blood, including red blood cells, white blood cells, and platelets. It can help to identify infections or other conditions that may be affecting wound healing.
- C-reactive protein (CRP): The CRP test measures protein levels in the blood in response to inflammation. Elevated levels of CRP may indicate infection or inflammation in the body.
- Blood cultures: Blood cultures are tests that can identify the presence of bacteria in the bloodstream, which can help to diagnose and treat infections.
- Wound culture: A wound culture is a test that involves taking a sample of the wound tissue or discharge and testing it for the presence of bacteria or other organisms contributing to the non-healing wound.
Laboratory tests can provide important information about underlying conditions contributing to non-healing foot wounds. By identifying these conditions, healthcare providers can develop personalized treatment plans that address the underlying causes of the injury and promote healing.
Strategies for Promoting Wound Healing
Effective wound healing strategies aim to address the underlying causes of the non-healing foot wound and promote optimal conditions for healing. Here are some methods that may be used to promote wound healing:
- Wound debridement: Debridement involves removing dead or damaged tissue from the wound to promote healing. This can be done using surgical techniques, such as sharp debridement or maggot therapy, or topical agents, such as enzymes or hydrogels.
- Dressings: Dressings can protect the wound from infection and promote healing. Different types of sauces may be used depending on the type and severity of the wound, and healthcare providers may need to change dressings regularly to monitor healing progress.
- Topical medications: Topical medications, such as antimicrobial agents or growth factors, may be applied directly to the wound to promote healing and prevent infection.
- Compression therapy: Compression therapy can be used to improve circulation in the affected foot and reduce swelling, which can promote healing. Different types of compression therapy, such as bandages or compression stockings, may be used depending on the individual’s specific needs and circumstances.
- Offloading: Offloading involves taking pressure off the affected foot to promote healing. This can be done using specialized shoes, braces, crutches, or other assistive devices to reduce weight bearing on the affected foot.
- Addressing underlying medical conditions: Addressing underlying medical conditions, such as diabetes or peripheral arterial disease, is essential for promoting wound healing. This may involve managing blood sugar levels, controlling blood pressure, or treating underlying infections or inflammation.
- Nutritional support: Adequate nutrition is essential for promoting wound healing. Healthcare providers may recommend dietary changes or nutritional supplements to ensure the body has healing nutrients.
Effective wound healing strategies typically involve a multidisciplinary approach that consists of a team of healthcare providers, including wound care specialists, podiatrists, and vascular surgeons. By working together and utilizing appropriate wound care techniques and strategies, healthcare providers can promote healing and reduce the risk of complications in people with non-healing foot wounds.
Wound cleaning and debridement
Wound cleaning and debridement are essential steps in managing non-healing foot wounds. These procedures involve removing dead or damaged tissue from the damage and cleaning the wound to promote healing.
Here are some of the critical steps involved in wound cleaning and debridement:
- Cleaning the wound: Before debridement, the damage must be cleaned to remove any debris or bacteria that may be present. This may involve rinsing the wound with saline solution or using other cleaning agents to remove dead tissue or foreign material.
- Debridement: Debridement involves removing dead or damaged tissue from the wound to promote healing. Different types of debridement may be used depending on the type and severity of the wound, including sharp debridement, mechanical debridement, and enzymatic debridement.
- Dressing the wound: After debridement, the damage is typically dressed to protect it from infection and promote healing. Different types of dressings may be used depending on the type and severity of the wound, and healthcare providers may need to change dressings regularly to monitor healing progress.
- Pain management: Debridement and wound cleaning procedures can be painful, so healthcare providers may use local anaesthesia or systemic pain medication to help manage pain.
Effective wound cleaning and debridement are essential for promoting healing and reducing the risk of complications in people with non-healing foot wounds. Healthcare providers must use appropriate techniques and strategies to ensure that wound cleaning and debridement are done safely and effectively while minimizing pain and discomfort for the affected individual.
Moist wound healing and dressings
Moist wound healing is a technique that involves keeping the wound bed moist and hydrated to promote healing. This contrasts dry wound healing, which allows the wound to dry out and form a scab. Moist wound healing is typically preferred for non-healing foot wounds because it can promote faster healing and reduce the risk of infection.
Here are some of the critical benefits of moist wound healing:
- Faster healing: Moist wound healing promotes speedier recovery by creating an optimal environment for new tissue growth.
- Reduced scarring: Moist wound healing can help reduce scarring by promoting new tissue growth.
- Reduced pain: Moist wound healing can help to reduce pain and discomfort associated with non-healing foot wounds.
- Reduced risk of infection: Moist wound healing can help to reduce the risk of disease by promoting a healthy wound bed and reducing the risk of bacteria and other pathogens.
Moist wound healing is typically achieved through the use of dressings that are designed to keep the wound bed moist and hydrated. Many different types of dressings are available, each with unique properties and benefits. Some common types of sauces used for moist wound healing include:
- Hydrocolloid dressings: These are made of a gel-like material that absorbs excess fluid from the wound while maintaining a moist environment.
- Hydrogel dressings: These are made of water or glycerin and are designed to keep the wound bed moist and hydrated.
- Foam dressings: These are designed to absorb excess fluid from the wound while maintaining a moist environment.
- Alginate dressings: These are made of seaweed and are designed to absorb excess fluid while maintaining a moist environment.
Effective use of dressings for moist wound healing is essential for promoting healing and reducing the risk of complications in people with non-healing foot wounds. Healthcare providers can help to determine the best type of dressing for the individual’s specific needs and circumstances. They can guide how to apply and change dressings to promote healing properly.
Offloading and pressure redistribution
Offloading and pressure redistribution are essential strategies for promoting healing in non-healing foot wounds, particularly in individuals with diabetes or peripheral arterial disease. These strategies involve reducing pressure on the affected foot to promote healing and prevent further damage.
Here are some of the critical offloading and pressure redistribution strategies that may be used:
- Custom shoes or braces: Healthcare providers may prescribe custom shoes or braces to reduce pressure on the affected foot and promote healing. These devices are designed to redistribute pressure away from the wound site and can help to improve healing outcomes.
- Casts or splints: In some cases, healthcare providers may use casts or splints to immobilize the affected foot and reduce pressure on the wound site.
- Crutches or other assistive devices: Crutches or other assistive devices may reduce weight bearing on the affected foot and promote healing.
- Pressure relief insoles or pads: Pressure relief insoles or pads may reduce pressure on specific foot areas and promote healing.
Effective offloading and pressure redistribution strategies can help promote healing and reduce the risk of complications in people with non-healing foot wounds. Healthcare providers can help determine the best plan for the individual’s specific needs and circumstances and provide guidance on using these strategies to promote healing properly.
Infection management and antibiotic therapy
Infection management and antibiotic therapy are essential components of the management of non-healing foot wounds. Infections can delay wound healing, increase the risk of complications, and even lead to sepsis, which can be life-threatening.
Here are some of the key strategies that may be used for infection management and antibiotic therapy in non-healing foot wounds:
- Wound culture: A wound culture may determine the type of bacteria present in the wound and the appropriate antibiotic to use.
- Antibiotic therapy may treat bacterial infections contributing to non-healing foot wounds. Different antibiotics may be used depending on the type and severity of the infection.
- Topical antibiotics: Topical antibiotics may be used to treat localized infections and prevent the spread of bacteria.
- Debridement: Debridement can help to remove bacteria and reduce the risk of infection.
- Surgical intervention: In some cases, surgical intervention may be necessary to remove infected tissue or drainage from an abscess.
- Infection control: Infection control measures may be used to prevent the spread of infection, such as hand hygiene and wearing gloves when changing wound dressings.
It is important to note that antibiotic therapy should be used judiciously to prevent the development of antibiotic-resistant bacteria. Healthcare providers will carefully evaluate the need for antibiotic therapy and select the appropriate antibiotic based on wound culture results and other factors.
Effective infection management and antibiotic therapy can help to promote healing and prevent complications in people with non-healing foot wounds. Healthcare providers can help determine the best strategy for the individual’s specific needs and circumstances and provide guidance on how to use these strategies to promote healing properly.
Vascular interventions (angioplasty, bypass surgery)
Vascular interventions such as angioplasty and bypass surgery may be recommended for people with non-healing foot wounds due to peripheral arterial disease. These interventions aim to improve blood flow to the affected foot and promote healing.
Here are some of the critical vascular interventions that may be used:
- Angioplasty: Angioplasty is a minimally invasive procedure that involves inserting a tiny balloon into the affected artery and inflating it to widen the highway and improve blood flow. Sometimes, a stent (a small metal mesh tube) may be inserted to keep the artery open.
- Bypass surgery involves creating a new path for blood flow around a blocked or narrowed artery. This is typically done using a graft (a vein or synthetic tubing) to bypass the secured area.
- Endarterectomy: Endarterectomy is a surgical procedure that involves removing the inner lining of a blocked or narrowed artery to improve blood flow.
Vascular interventions can effectively improve blood flow to the affected foot and promote healing in people with non-healing foot wounds. However, these interventions are typically reserved for people with severe peripheral arterial disease who have not responded to other treatments. It is essential for healthcare providers to carefully evaluate the need for vascular interventions and consider the potential risks and benefits before recommending these procedures.
In addition to vascular interventions, it is essential to address underlying medical conditions, such as diabetes and hypertension, to promote healing and reduce the risk of complications. A comprehensive approach that includes a combination of strategies, such as wound debridement, offloading, infection management, and vascular interventions, can help to promote healing and improve outcomes in people with non-healing foot wounds.
Advanced wound care therapies (growth factors, skin substitutes)
Advanced wound care therapies may be used to manage non-healing foot wounds to promote healing and improve outcomes. These therapies include growth factors, skin substitutes, and other biologic agents.
Here are some of the critical advanced wound care therapies that may be used:
- Growth factors: Growth factors are naturally occurring proteins that play a role in wound healing. They can be applied topically or injected directly into the wound to promote healing.
- Skin substitutes: Skin substitutes are products designed to replace or supplement the natural skin in the affected area. These products may be made of natural or synthetic materials and can help to promote healing and reduce scarring.
- Cellular therapy involves using cells, such as stem cells or platelet-rich plasma (PRP), to promote healing in non-healing foot wounds.
- Extracorporeal shock wave therapy: Extracorporeal shock wave therapy (ESWT) is a non-invasive therapy that uses shock waves to stimulate healing in non-healing foot wounds.
- Negative pressure wound therapy: Negative pressure wound therapy (NPWT) involves the application of negative pressure to the wound site to promote healing and reduce the risk of infection.
These advanced wound care therapies are typically reserved for people with non-healing foot wounds that have not responded to other treatments. Healthcare providers will carefully evaluate the need for these therapies and select the appropriate medicine based on the individual’s specific needs and circumstances.
It is important to note that these advanced wound care therapies may not be covered by insurance and can be expensive. Healthcare providers can guide the availability and cost of these therapies and help individuals make informed decisions about their treatment options.
Hyperbaric oxygen therapy
Hyperbaric oxygen therapy (HBOT) is a treatment option for non-healing foot wounds that involves breathing in pure oxygen while inside a pressurized chamber. This therapy can increase the amount of oxygen delivered to the wound site, promoting healing and reducing the risk of infection.
Here are some of the critical benefits of hyperbaric oxygen therapy:
- Improved tissue oxygenation: Hyperbaric oxygen therapy can increase the amount of oxygen delivered to the wound site, which can help promote healing and reduce the risk of infection.
- Increased blood flow: HBOT can stimulate the growth of new blood vessels in the affected area, improving blood flow and promoting healing.
- Reduced inflammation: HBOT can help to reduce inflammation and swelling in the affected area, which can help to promote healing and reduce pain.
- Enhanced antibiotic effectiveness: HBOT can improve the effectiveness of antibiotics by increasing oxygen levels in the affected area, which can enhance bacterial killing.
Hyperbaric oxygen therapy is typically used as an adjunct therapy with other treatments, such as wound debridement, offloading, and infection management. It may be recommended for non-healing foot wounds due to diabetes, peripheral arterial disease, or other underlying conditions.
It is important to note that hyperbaric oxygen therapy may not suit everyone. Healthcare providers will carefully evaluate the need for this therapy and consider the potential risks and benefits before recommending it. Additionally, hyperbaric oxygen therapy can be expensive. It may not be covered by insurance, so healthcare providers can provide guidance on the availability and cost of this therapy and help individuals make informed decisions about their treatment options.
Negative pressure wound therapy
Negative pressure wound therapy (NPWT) is a treatment option for non-healing foot wounds that involve applying negative pressure to the wound site using a specialized device. This therapy can help promote healing by removing excess fluid and promoting healthy tissue growth.
Here are some of the critical benefits of negative pressure wound therapy:
- Improved wound healing: Negative pressure wound therapy can help promote healing by removing excess fluid from the wound site and promoting healthy tissue growth.
- Reduced risk of infection: NPWT can help to reduce the risk of disease by removing excess fluid and reducing bacterial colonization in the wound.
- Reduced inflammation: NPWT can help to reduce inflammation and swelling in the affected area, which can help to promote healing and reduce pain.
- Easy application: NPWT can be easily applied to the wound site using a specialized device, reducing the need for frequent dressing changes and improving patient comfort.
Negative pressure wound therapy is typically used as an adjunct therapy with other treatments, such as wound debridement, offloading, and infection management. It may be recommended for non-healing foot wounds due to diabetes, peripheral arterial disease, or other underlying conditions.
It is important to note that negative pressure wound therapy may not be suitable for everyone. Healthcare providers will carefully evaluate the need for this therapy and consider the potential risks and benefits before recommending it. Additionally, negative pressure wound therapy can be expensive. It may not be covered by insurance, so healthcare providers can provide guidance on the availability and cost of this therapy and help individuals make informed decisions about their treatment options.
Importance of Comprehensive Foot Care
Comprehensive foot care is essential for non-healing foot wounds, particularly those with underlying medical conditions such as diabetes, peripheral arterial disease, or venous insufficiency. Proper foot care can help to promote healing, prevent complications, and improve overall quality of life.
Here are some of the critical elements of comprehensive foot care:
- Regular foot exams: Regular foot exams can help to detect early signs of foot problems and prevent complications. Healthcare providers can perform a comprehensive foot exam and guide proper foot care.
- Proper wound care: Proper wound care is essential for promoting healing and preventing infection. This may include cleaning the wound, applying dressings, and using offloading and pressure redistribution strategies.
- Blood glucose control: Blood glucose control is essential for people with diabetes to prevent complications and promote healing. Healthcare providers can guide proper blood glucose monitoring and management.
- Vascular assessment and management: Vascular assessment and management are essential for people with peripheral arterial disease or venous insufficiency. This may include vascular interventions, such as angioplasty or bypass surgery, to improve blood flow to the affected foot.
- Education and self-care: Education and self-care are essential for maintaining proper foot health. Healthcare providers can guide appropriate foot care, including footwear, regular foot exams, and wound care.
- Multidisciplinary care: Multidisciplinary care involves a team-based approach to foot care that may include healthcare providers such as podiatrists, wound care specialists, vascular specialists, and endocrinologists. This approach can provide comprehensive care and improve outcomes for people with non-healing foot wounds.
Comprehensive foot care is essential for promoting healing, preventing complications, and improving the overall quality of life in people with non-healing foot wounds. Healthcare providers can guide proper foot care and help individuals develop a personalized care plan that meets their needs and circumstances.
Regular foot inspections and self-care practices
Regular foot inspections and self-care practices are essential elements of comprehensive foot care for people with non-healing foot wounds, particularly those with underlying medical conditions such as diabetes, peripheral arterial disease, or venous insufficiency. These practices can help to detect early signs of foot problems and prevent complications.
Here are some of the critical foot inspection and self-care practices:
- Daily foot inspections: Daily foot inspections can help to detect early signs of foot problems, such as cuts, blisters, or changes in skin colour or temperature. Inspecting the feet thoroughly, including between the toes, can help to identify any potential issues that may require medical attention.
- Proper footwear: Proper footwear protects the feet and prevents foot problems. This may include wearing shoes that fit properly, provide adequate support, and have a wide-toe box. People with non-healing foot wounds may require specialized footwear to prevent pressure and reduce the risk of injury.
- Proper nail care: Proper nail care prevents infections and other foot problems. This may include keeping the nails trimmed and filed, avoiding cutting the nails too short and avoiding using sharp objects to clean the nails.
- Moisturizing: Moisturizing the feet can help prevent dryness and cracking, leading to foot problems. Regular moisturizing cream or lotion can help keep the skin soft and supple.
- Blood glucose control: Blood glucose control is essential for people with diabetes to prevent complications and promote healing. Monitoring blood glucose regularly and following a healthy diet and exercise routine can help to maintain proper blood glucose levels.
Regular foot inspections and self-care practices are essential for maintaining proper foot health and preventing complications in people with non-healing foot wounds. Healthcare providers can guide appropriate foot care and help individuals develop a personalized care plan that meets their needs and circumstances.
Proper footwear selection
Proper footwear selection is essential to comprehensive foot care for people with non-healing foot wounds. Proper footwear can help to reduce pressure on the affected foot, protect the foot from injury, and prevent foot problems.
Here are some of the critical factors to consider when selecting proper footwear:
- Fit: Proper fit is essential for preventing foot problems. Shoes should fit comfortably without rubbing or causing pressure points. The toe box should be wide enough for proper toe movement, and the heel should fit snugly without slipping.
- Support: Proper support can help to reduce pressure on the affected foot and prevent foot problems. Shoes with a low heel and good arch support can help to distribute weight evenly across the foot and reduce pressure points.
- Material: The material of the shoe is also essential for preventing foot problems. Shoes made of breathable materials, such as leather or mesh, can help to prevent moisture buildup and reduce the risk of infection.
- Design: Shoes with a wide, deep toe box and a flexible sole can help to reduce pressure on the affected foot and prevent foot problems. Shoes with adjustable straps or laces can also help to ensure a proper fit.
- Activity level: The type of shoe needed may also depend on the individual’s activity level. More active people may require shoes with more cushioning and support, while those who are less active may require shoes with less support.
People with non-healing foot wounds must work with their healthcare provider to select proper footwear that meets their needs and circumstances. Specialized shoes or orthotics may be necessary to reduce pressure on the affected foot and prevent complications.
Regular podiatric care and monitoring
Regular podiatric care and monitoring are essential to comprehensive foot care for people with non-healing foot wounds. Podiatric care involves regular visits with a podiatrist specializing in diagnosing and treating foot and ankle problems.
Here are some of the key benefits of regular podiatric care and monitoring:
- Early detection of foot problems: Regular visits with a podiatrist can help to detect early signs of foot problems, such as non-healing wounds, infections, or changes in skin colour or temperature.
- Preventative care: Podiatrists can guide proper foot care, including adequate footwear selection, self-care practices, and regular foot inspections. This can help to prevent foot problems from occurring in the first place.
- Treatment and management of foot problems: Podiatrists can diagnose and treat various foot problems, including non-healing foot wounds, infections, and neuropathy. They can also develop a personalized treatment plan that meets the individual’s needs and circumstances.
- Referral to other healthcare providers: Podiatrists can refer individuals to other healthcare providers, such as wound care specialists or vascular specialists, to provide comprehensive care.
Regular podiatric care and monitoring are essential for maintaining proper foot health and preventing complications in people with non-healing foot wounds. Healthcare providers can guide appropriate foot care and help individuals develop a personalized care plan that meets their needs and circumstances.
Education on foot hygiene and injury prevention
Education on foot hygiene and injury prevention is essential to comprehensive foot care for people with non-healing foot wounds. Proper education can help individuals to develop healthy habits and reduce the risk of foot problems.
Here are some of the critical elements of education on foot hygiene and injury prevention:
- Foot hygiene: Proper foot hygiene is essential for preventing problems such as infections and non-healing wounds. Healthcare providers can guide proper foot washing, drying, and moisturizing.
- Self-care practices: Self-care practices, such as daily foot inspections, proper nail care, and the use of appropriate footwear, can help to prevent foot problems and detect early signs of foot problems.
- Injury prevention: Injury prevention is essential for reducing the risk of foot problems. This may include wearing appropriate footwear during physical activity, avoiding walking barefoot, and using caution when using sharp objects.
- Blood glucose control: Proper blood glucose control is essential for people with diabetes to prevent foot problems and promote healing. Healthcare providers can guide proper blood glucose monitoring and management.
- Proper wound care: Proper wound care is essential for promoting healing and preventing infection. Healthcare providers can guide good wound cleaning, dressing, and offloading.
Education on foot hygiene and injury prevention can help individuals to develop healthy habits and reduce the risk of foot problems. Healthcare providers can guide proper foot care and help individuals develop a personalized care plan that meets their needs and circumstances.
Blood sugar control and diabetes management
Blood sugar control and diabetes management are essential elements of comprehensive foot care for people with non-healing foot wounds who have diabetes. Proper blood sugar control can help to prevent foot problems and promote healing.
Here are some of the critical elements of blood sugar control and diabetes management:
- Blood glucose monitoring: Regular blood glucose monitoring can help to detect changes in blood sugar levels and identify the need for adjustments in diabetes management.
- Medications: Oral medications or insulin may be prescribed to help control blood sugar levels.
- Diet and exercise: A healthy diet and regular exercise can help to maintain proper blood sugar levels and reduce the risk of foot problems.
- Regular healthcare visits: Regular healthcare visits can help to monitor blood sugar levels and provide guidance on proper diabetes management.
- Foot care: Proper foot care, including daily foot inspections, proper footwear, and regular podiatric care, can help to prevent foot problems and promote healing.
It is essential for people with non-healing foot wounds who have diabetes to work with their healthcare provider to develop a personalized diabetes management plan that meets their specific needs and circumstances. Proper blood sugar control and diabetes management can help to prevent foot problems and promote healing, reducing the risk of complications and improving the overall quality of life.
Multidisciplinary Approach to Wound Management
A multidisciplinary approach to wound management is essential for people with non-healing foot wounds. This approach involves a team-based approach to care that includes healthcare providers from various disciplines, such as podiatrists, wound care specialists, vascular specialists, and endocrinologists.
Here are some of the critical benefits of a multidisciplinary approach to wound management:
- Comprehensive care: A multidisciplinary approach to wound management provides comprehensive care that addresses the various factors that contribute to non-healing foot wounds, such as diabetes, peripheral arterial disease, and venous insufficiency.
- Personalized treatment: A multidisciplinary approach allows for a customized treatment plan that meets the individual’s needs and circumstances.
- Improved outcomes: A multidisciplinary approach has been shown to improve outcomes in people with non-healing foot wounds, such as reducing the risk of complications and promoting healing.
- Collaborative approach: A multidisciplinary approach involves a collaborative approach to care, with healthcare providers working together to provide coordinated and effective care.
- Education and support: A multidisciplinary approach can provide education and support for individuals with non-healing foot wounds and their caregivers, helping them to develop healthy habits and reduce the risk of complications.
A multidisciplinary approach to wound management is essential for promoting healing, preventing complications, and improving the overall quality of life in people with non-healing foot wounds. Healthcare providers can guide proper wound management and help individuals develop a personalized care plan that meets their needs and circumstances.
Collaboration between healthcare professionals (physicians, podiatrists, wound care specialists)
Collaboration between healthcare professionals, such as physicians, podiatrists, and wound care specialists, is essential for providing comprehensive care for people with non-healing foot wounds. This collaboration involves a team-based approach to care that involves sharing information, coordinating treatment, and working together to address the various factors contributing to non-healing foot wounds.
Here are some of the key benefits of collaboration between healthcare professionals:
- Comprehensive care: Collaboration between healthcare professionals can provide comprehensive care that addresses the various factors that contribute to non-healing foot wounds, such as diabetes, peripheral arterial disease, and venous insufficiency.
- Personalized treatment: Collaboration between healthcare professionals allows for a customized treatment plan that meets the individual’s needs and circumstances.
- Improved outcomes: Collaboration between healthcare professionals has been shown to improve outcomes in people with non-healing foot wounds, such as reducing the risk of complications and promoting healing.
- Coordination of care: Collaboration between healthcare professionals allows care coordination across different specialities, ensuring that all aspects of care are addressed.
- Education and support: Collaboration between healthcare professionals can provide education and support for individuals with non-healing foot wounds and their caregivers, helping them to develop healthy habits and reduce the risk of complications.
Collaboration between healthcare professionals is essential for promoting healing, preventing complications, and improving the overall quality of life in people with non-healing foot wounds. Healthcare providers can work together to develop a personalized care plan that meets the individual’s specific needs and circumstances.
Role of physical therapists and occupational therapists
Physical and occupational therapists can be essential in managing non-healing foot wounds. They can help individuals with non-healing foot wounds to improve mobility, reduce pain, and prevent complications.
Here are some of the critical roles of physical therapists and occupational therapists in the management of non-healing foot wounds:
- Mobility and gait training: Physical therapists can provide mobility and gait training to help individuals with non-healing foot wounds to improve their ability to walk and move around. This may involve exercises to improve strength, balance, flexibility, and assistive devices like crutches or walkers.
- Wound care: Occupational therapists can provide wound care education and training, including proper cleaning and dressing of wounds, to help individuals with non-healing foot wounds to prevent infection and promote healing.
- Pressure ulcer prevention: Physical and occupational therapists can provide education on pressure ulcer prevention, including proper positioning and pressure relief devices, to help reduce the risk of pressure ulcers in individuals with non-healing foot wounds.
- Assistive devices: Physical therapists and occupational therapists can recommend and assist in the use of assistive devices, such as orthotics, braces, or prosthetics, to help individuals with non-healing foot wounds to reduce pressure on the affected foot and prevent complications.
- Education and support: Physical and occupational therapists can educate and support individuals with non-healing foot wounds and their caregivers, helping them develop healthy habits and reduce the risk of complications.
Physical and occupational therapists can play an essential role in managing non-healing foot wounds, helping to improve mobility, reducing pain, preventing complications, and improving the overall quality of life. Healthcare providers can work together to develop a personalized care plan that includes physical and occupational therapists’ input and expertise.
Nutrition counselling for optimal wound healing
Nutrition counselling is essential to comprehensive care for people with non-healing foot wounds. Proper nutrition can help to promote healing and reduce the risk of complications.
Here are some of the critical factors to consider in nutrition counselling for optimal wound healing:
- Protein: Protein is essential for wound healing. It provides the building blocks for new tissue growth and repair. Healthcare providers may recommend increasing protein intake through dietary sources, such as lean meats, fish, eggs, and legumes, or protein supplements.
- Vitamins and minerals: Vitamins and minerals are essential in wound healing. In particular, vitamins A, C, and E, as well as zinc and iron, are necessary for tissue growth and repair. Healthcare providers may recommend increasing the intake of foods that are rich in these vitamins and minerals or may recommend supplements.
- Hydration: Proper hydration is essential for wound healing. Healthcare providers may recommend increasing fluid intake to help promote healing and prevent dehydration.
- Caloric intake: Proper caloric information is also essential for wound healing. Healthcare providers may recommend increasing caloric intake to help provide the energy and nutrients needed for tissue growth and repair.
- Weight management: In some cases, weight management may also be necessary for optimal wound healing. Healthcare providers may recommend weight loss or management strategies to reduce pressure on the affected foot and promote healing.
Nutrition counselling can be essential in promoting healing and preventing complications in people with non-healing foot wounds. Healthcare providers can guide proper nutrition and help individuals develop a personalized nutrition plan that meets their needs and circumstances.
Psychological support and addressing emotional challenges
Psychological support and addressing emotional challenges are essential to comprehensive care for people with non-healing foot wounds. Non-healing foot wounds can be a source of stress, anxiety, and depression, hurting the overall quality of life and the healing process.
Here are some of the critical elements of psychological support and addressing emotional challenges:
- Mental health screening: Healthcare providers may conduct mental health screenings to assess for symptoms of anxiety, depression, or other mental health conditions.
- Counselling: Counseling, including cognitive-behavioural therapy, can help individuals to develop coping strategies and address emotional challenges related to non-healing foot wounds.
- Support groups: Support groups can provide a sense of community and help individuals to feel less isolated. Support groups can also provide education on wound management and coping strategies.
- Education and communication: Healthcare providers can educate on non-healing foot wounds and address individuals’ concerns or fears. Clear communication and education can help to reduce anxiety and promote healing.
- Family support: Family members and caregivers can be essential in providing emotional support and helping with wound care.
Psychological support and addressing emotional challenges are essential to comprehensive care for people with non-healing foot wounds. Healthcare providers can provide guidance and resources for addressing emotional difficulties, including counselling and support groups. Individuals need to seek help if they are experiencing emotional challenges related to non-healing foot wounds, as addressing these challenges can improve the overall quality of life and the healing process.
Lifestyle Modifications and Prevention Strategies
Lifestyle modifications and prevention strategies can help to reduce the risk of non-healing foot wounds and promote healing in individuals who have already developed non-healing foot wounds. Here are some essential lifestyle modifications and prevention strategies:
- Blood glucose control: Proper blood glucose control is essential for preventing and managing non-healing foot wounds in individuals with diabetes. Healthcare providers can guide proper blood glucose monitoring and management.
- Foot hygiene: Proper foot hygiene, including daily foot inspections, can help to prevent infections and detect early signs of foot problems.
- Proper footwear: Proper footwear can help to reduce the risk of foot injuries and pressure ulcers. Individuals should choose shoes that fit correctly and comfortably, with adequate support and cushioning.
- Regular physical activity: Regular physical activity can help to improve circulation, reduce the risk of obesity and peripheral arterial disease, and promote healing.
- Healthy diet: A healthy diet, rich in protein, vitamins, and minerals, can help to provide the nutrients needed for wound healing and overall health.
- Smoking cessation: Smoking can impair circulation and slow the healing process. Individuals who smoke should quit smoking to reduce the risk of non-healing foot wounds and promote healing.
- Regular podiatric care: Regular podiatric care can help to detect early signs of foot problems and prevent complications.
Lifestyle modifications and prevention strategies can help to reduce the risk of non-healing foot wounds and promote healing in individuals who have already developed non-healing foot wounds. Healthcare providers can provide guidance and resources for implementing lifestyle modifications and prevention strategies that meet the individual’s needs and circumstances.
Smoking cessation
Smoking cessation is a crucial lifestyle modification for people with non-healing foot wounds. Smoking can impair circulation, reduce the oxygen supply to tissues, and slow the healing process, increasing the risk of complications and delaying healing.
Here are some of the critical benefits of smoking cessation for people with non-healing foot wounds:
- Improved circulation: Smoking cessation can help improve circulation, which is essential for wound healing. Improved circulation can help to deliver oxygen and nutrients to the affected foot, promoting healing.
- Reduced inflammation: Smoking can increase inflammation in the body, impairing wound healing. Smoking cessation can help to reduce inflammation and promote healing.
- Reduced risk of infection: Smoking can increase the risk of disease, which can delay healing and increase the risk of complications. Smoking cessation can help to reduce the risk of illness and promote healing.
- Improved overall health: Smoking cessation can improve overall health and reduce the risk of other health problems like heart disease and lung disease.
- Improved quality of life: Smoking cessation can improve the overall quality of life, including physical health, emotional well-being, and social interactions.
Smoking cessation is a crucial lifestyle modification for people with non-healing foot wounds. Healthcare providers can provide resources and support for smoking cessation, including nicotine replacement therapy, counselling, and support groups. It is essential for individuals with non-healing foot wounds who smoke to quit smoking to reduce the risk of complications and promote healing.
A healthy diet and weight management
A healthy diet and weight management are essential lifestyle modifications for people with non-healing foot wounds. A healthy diet can help to provide the nutrients needed for wound healing and overall health, while weight management can help to reduce pressure on the affected foot and promote healing.
Here are some of the critical benefits of a healthy diet and weight management for people with non-healing foot wounds:
- Proper nutrition: A healthy diet can help to provide the nutrients needed for wound healing, including protein, vitamins, and minerals. Healthcare providers can guide adequate nutrition and help individuals develop a personalized nutrition plan that meets their needs and circumstances.
- Weight management: Weight management can help to reduce pressure on the affected foot and promote healing. Healthcare providers can guide proper weight management strategies, including diet and exercise.
- Reduced inflammation: A healthy diet can help to reduce inflammation in the body, which can impair wound healing.
- Improved circulation: Weight management can help to improve circulation, which is essential for wound healing.
- Improved overall health: A healthy diet and weight management can improve overall health and reduce the risk of other health problems, such as heart disease and diabetes.
A healthy diet and weight management are essential lifestyle modifications for people with non-healing foot wounds. Healthcare providers can provide guidance and resources for implementing healthy eating and weight management strategies that meet the individual’s needs and circumstances.
Regular exercise to improve circulation
Regular exercise is a crucial lifestyle modification for people with non-healing foot wounds, as it can help to improve circulation and promote healing. Exercise can help to increase blood flow to the affected foot, which can help to deliver oxygen and nutrients to the tissues and promote healing.
Here are some of the key benefits of regular exercise for people with non-healing foot wounds:
- Improved circulation: Regular exercise can help to improve circulation, which is essential for wound healing.
- Increased mobility: Regular exercise can help to improve mobility and range of motion, which can help to reduce the risk of falls and improve the overall quality of life.
- Reduced inflammation: Regular exercise can help reduce inflammation in the body, impairing wound healing.
- Improved overall health: Regular exercise can improve overall health and reduce the risk of other health problems like heart disease and diabetes.
Here are some essential considerations for exercise in individuals with non-healing foot wounds:
- Consultation with a healthcare provider: Individuals with non-healing foot wounds should consult with their healthcare provider before starting an exercise program.
- Proper footwear: Proper footwear is essential for exercise in individuals with non-healing foot wounds. Individuals should choose shoes that fit correctly and provide adequate support and cushioning.
- Proper exercise selection: Healthcare providers can guide good exercise selection and modifications for individuals with non-healing foot wounds based on their specific needs and circumstances.
Regular exercise is a crucial lifestyle modification for people with non-healing foot wounds. Healthcare providers can provide guidance and resources for implementing an exercise program that meets the individual’s needs and circumstances.
Stress management techniques
Stress management techniques are essential for people with non-healing foot wounds, as non-healing foot wounds can be a source of stress, anxiety, and depression. Stress can hurt the overall quality of life and the healing process. Here are some stress management techniques that may be helpful:
- Relaxation techniques: Relaxation techniques, such as deep breathing, meditation, and guided imagery, can help to reduce stress and promote healing.
- Exercise: Regular exercise can help to reduce stress and promote healing. Exercise can also help to improve circulation and reduce inflammation.
- Support groups: Support groups can provide a sense of community and help individuals to feel less isolated. Support groups can also provide education on wound management and coping strategies.
- Counselling: Counseling, including cognitive-behavioural therapy, can help individuals to develop coping strategies and address emotional challenges related to non-healing foot wounds.
- Time management: Proper time management can help to reduce stress and promote healing. Individuals can prioritize tasks and delegate responsibilities to minimize stress and focus on wound care.
- Mindfulness: Mindfulness techniques like breathing and movement can help reduce stress and promote healing.
Stress management techniques are essential to comprehensive care for people with non-healing foot wounds. Healthcare providers can provide guidance and resources for stress management techniques that meet the individual’s needs and circumstances.
Self-care practices for foot hygiene and protection
Self-care practices for foot hygiene and protection are essential for individuals with non-healing foot wounds, as they can help to prevent infections and reduce the risk of further injury. Here are some self-care practices that may be helpful:
- Daily foot inspections: Individuals should inspect their feet daily for any signs of redness, swelling, or sores. Any changes should be reported to a healthcare provider.
- Proper foot hygiene: Proper foot hygiene, including daily washing with mild soap and water, can help to prevent infections.
- Moisturizing: Moisturizing the feet daily can help prevent dryness and cracking, increasing the risk of infection.
- Proper footwear: Proper footwear is essential for individuals with non-healing foot wounds. Shoes should fit properly and provide adequate support and cushioning.
- Avoiding barefoot walking: Individuals with non-healing foot wounds should avoid walking barefoot, as this can increase the risk of injury and infection.
- Avoiding extreme temperatures: Individuals with non-healing foot wounds should avoid exposure to extreme temperatures, which can increase the risk of injury and infection.
- Protecting the feet: Individuals with non-healing foot wounds should protect themselves from injury by wearing shoes that fit correctly and avoiding high-risk activities.
Self-care practices for foot hygiene and protection are essential to comprehensive care for people with non-healing foot wounds. Healthcare providers can provide guidance and resources for self-care courses that meet the individual’s needs and circumstances.
The Importance of Timely Intervention and Seeking Medical Help
Timely intervention and seeking medical help are crucial for individuals with non-healing foot wounds. Non-healing foot wounds can lead to severe complications and even amputation if not treated promptly and effectively.
Here are some reasons why timely intervention and seeking medical help are essential:
- Early detection of problems: Timely intervention can help to detect and address issues early before they become more severe and difficult to treat.
- Effective wound management: Timely intervention can help to implement effective wound management strategies, such as wound cleaning, debridement, and dressings.
- Prevention of complications: Timely intervention can help to prevent complications associated with non-healing foot wounds, such as infection, gangrene, and amputation.
- Multidisciplinary approach: Timely intervention can facilitate an interdisciplinary approach to wound management, involving healthcare providers from various disciplines who can collaborate to provide comprehensive care.
- Improved quality of life: Timely intervention can help to improve the overall quality of life by promoting healing and reducing the risk of complications.
Individuals with non-healing foot wounds must seek medical help promptly if they experience any changes or problems with their feet. Healthcare providers can provide guidance and resources for effective wound management, including wound cleaning, debridement, dressings, and other necessary interventions.
Recognizing signs of infection or worsening wound condition
Recognizing signs of infection or worsening wound condition is essential for individuals with non-healing foot wounds, as early detection can help to prevent complications and improve outcomes. Here are some signs to watch for:
- Redness and swelling around the wound
- Increased pain or tenderness around the wound
- Drainage from the injury that is thick, yellow, or green
- A foul odour coming from the wound
- Increased warmth around the wound
- Fever or chills
- Red streaks spreading from the wound
- Worsening wound conditions, such as increasing size or depth or lack of progress in healing
Individuals should seek medical attention promptly if any of these signs are present. Healthcare providers can evaluate the wound and determine if further intervention, such as antibiotic therapy or debridement, is needed. It is important to note that some signs of infection may not be immediately visible, so it is essential for individuals with non-healing foot wounds to maintain regular communication with their healthcare providers and report any changes or concerns promptly.
The Role of patient vigilance and prompt reporting
Patient vigilance and prompt reporting are crucial for individuals with non-healing foot wounds. Non-healing foot wounds can lead to severe complications if not monitored closely and treated promptly. Here are some reasons why patient vigilance and prompt reporting are essential:
- Early detection of problems: Patient vigilance can help to detect problems early before they become more severe and difficult to treat.
- Timely intervention: Prompt reporting can facilitate timely intervention and effective wound management, which can help to prevent complications and promote healing.
- Collaborative approach: Patient vigilance and prompt reporting can facilitate a collaborative approach to wound management, involving healthcare providers and patients working together to achieve optimal outcomes.
- Empowerment: Patient vigilance and prompt reporting can empower individuals with non-healing foot wounds to take an active role in their care and promote healing.
It is crucial for individuals with non-healing foot wounds to be vigilant in monitoring their injuries and to report any changes or concerns promptly to their healthcare providers. This may include daily foot inspections and regular communication with their healthcare team. Healthcare providers can provide guidance and resources for monitoring wounds, reporting changes, and working collaboratively with patients to achieve optimal outcomes.
The importance of regular follow-up appointments
Regular follow-up appointments are crucial for individuals with non-healing foot wounds. Follow-up appointments allow healthcare providers to monitor the healing process, adjust treatment plans as needed, and address any concerns or complications.
Here are some reasons why regular follow-up appointments are essential:
- Monitoring healing progress: Regular follow-up appointments allow healthcare providers to monitor the healing process and evaluate the effectiveness of wound management strategies.
- Adjusting treatment plans: Follow-up appointments allow healthcare providers to adjust treatment plans to optimize healing and prevent complications.
- Preventing complications: Regular follow-up appointments can help to avoid complications associated with non-healing foot wounds, such as infection and amputation.
- Collaborative approach: Follow-up appointments facilitate a collaborative approach to wound management, involving healthcare providers and patients working together to achieve optimal outcomes.
- Patient education: Follow-up appointments provide opportunities for patient education on wound care, foot hygiene, and injury prevention.
Individuals with non-healing foot wounds must attend all scheduled follow-up appointments and communicate any concerns or changes in their condition to their healthcare provider. By working collaboratively with their healthcare team, individuals can optimize healing and prevent complications associated with non-healing foot wounds.
When to seek immediate medical attention
Individuals with non-healing foot wounds should seek immediate medical attention if they experience any of the following:
- Signs of infection: Redness, swelling, warmth, drainage from the wound that is thick, yellow, or green, foul odour coming from the injury, and fever or chills.
- Worsening wound condition: Increasing pain, tenderness, wound size, or lack of progress in healing.
- New symptoms: New onset of pain, numbness, or tingling in the feet, or any other new symptoms that are concerning.
- Trauma or injury: Trauma or damage to the foot, including cuts, punctures, or burns.
- High fever or severe pain: High or severe pain is not relieved with over-the-counter pain medications.
If any of these symptoms or conditions are present, individuals should seek immediate medical attention by contacting their healthcare provider or going to the emergency room. Prompt medical attention can help to prevent complications and promote healing. Individuals with non-healing foot wounds must communicate openly with their healthcare providers and seek medical attention promptly if any changes or concerns arise.
Recap of the causes and complications of non-healing foot wounds
Non-healing foot wounds can be caused by a variety of factors, including:
- Diabetes: High blood sugar levels associated with diabetes can impair the body’s natural healing mechanisms.
- Peripheral arterial disease (PAD): PAD can lead to reduced blood flow to the feet, impairing healing.
- Venous insufficiency: Venous insufficiency can lead to blood pooling in the feet, impairing healing.
- Pressure ulcers: Prolonged pressure on the feet can cause pressure ulcers, which can be difficult to heal.
- Infection: Infection can impede the healing process and lead to further complications.
- Neuropathy: Neuropathy can lead to reduced sensation in the feet, increasing the risk of injury and impeding healing.
Complications associated with non-healing foot wounds include:
- Infection: Infection can spread to surrounding tissues and lead to serious complications, such as cellulitis, osteomyelitis, and sepsis.
- Gangrene and tissue necrosis: Gangrene and tissue necrosis can occur when insufficient blood flow to the feet, leading to amputation.
- Amputation: Non-healing foot wounds can lead to amputation if not treated promptly and effectively.
- Systemic infections and sepsis: Infection can spread to the bloodstream, leading to potentially life-threatening sepsis.
- Reduced quality of life: Non-healing foot wounds can be painful and limit mobility, leading to reduced quality of life.
Individuals with non-healing foot wounds must seek medical attention promptly, maintain regular follow-up appointments, and practice self-care techniques to promote healing and prevent complications.
Emphasis on the importance of early intervention and comprehensive wound management
Early intervention and comprehensive wound management are crucial for individuals with non-healing foot wounds. Early detection and prompt treatment can help to prevent complications, improve healing outcomes, and reduce the risk of amputation.
Comprehensive wound management involves a multidisciplinary approach, including healthcare providers from various disciplines working collaboratively to provide complete care. This may include wound cleaning and debridement, moist wound healing and dressings, offloading and pressure redistribution, infection management and antibiotic therapy, vascular interventions such as angioplasty or bypass surgery, and advanced wound care therapies such as growth factors and skin substitutes.
Individuals with non-healing foot wounds must seek medical attention promptly and maintain regular follow-up appointments to monitor the healing process and adjust treatment plans. Patients should also practice self-care techniques for foot hygiene and protection and follow a healthy lifestyle to improve circulation, manage blood sugar levels, and reduce the risk of complications.
Overall, early intervention and comprehensive wound management are essential for individuals with non-healing foot wounds to achieve optimal healing outcomes and prevent serious complications.
Encouragement for individuals with non-healing foot wounds to seek professional help
If you have non-healing foot wounds, it is important to seek professional help as soon as possible. Seeking professional help can help you to manage your injuries effectively and prevent serious complications.
It is common to feel hesitant or anxious about seeking professional help. Still, it is important to remember that healthcare providers are there to support and guide you through the healing process. They can provide expert guidance, resources, and interventions to help promote healing and prevent complications.
Remember, the sooner you seek professional help, the better your chances of achieving optimal healing outcomes. Don’t hesitate to contact your healthcare provider or wound care specialist for assistance. With the right care and support, you can take control of your wound healing and get back to enjoying a healthy, active life.
The significance of patient education, adherence to treatment plans, and prevention strategies
Patient education, adherence to treatment plans, and prevention strategies are essential for individuals with non-healing foot wounds to achieve optimal healing outcomes and prevent complications.
Patient education involves providing information and guidance on wound care, foot hygiene, and injury prevention. This may include instructions on how to clean and dress wounds, how to perform daily foot inspections, and how to select appropriate footwear. Patients should also receive education on the importance of blood sugar control, healthy lifestyle habits, and regular follow-up appointments.
Adherence to treatment plans is also crucial for wound healing. Patients should follow their healthcare provider’s recommendations, including wound care instructions, medication regimens, and lifestyle modifications. Adherence to treatment plans can optimize healing outcomes and prevent complications.
Prevention strategies are also important for individuals with non-healing foot wounds. This may include wearing appropriate footwear, maintaining good foot hygiene, managing blood sugar levels, avoiding smoking, and maintaining a healthy lifestyle. Prevention strategies can help to reduce the risk of further injury, infection, and complications.
In summary, patient education, adherence to treatment plans, and prevention strategies are all essential for individuals with non-healing foot wounds. By working closely with their healthcare providers, patients can optimize healing outcomes and achieve a better quality of life.