Renal Parenchymal Disease: Causes, Symptoms, Diagnosis, and Treatment
Renal parenchymal disease is a broad term encompassing various conditions affecting the functional tissue of the kidneys. These conditions can lead to impaired kidney function and, if left untreated, may progress to chronic kidney disease (CKD) or dnend-stage renal disease (ESRD). This comprehensive guide will explore the causes, symptoms, diagnosis, and treatment options for renal parenchymal disease. Understanding this condition is essential for healthcare professionals and individuals looking to enhance their knowledge of kidney health.
What is Renal Parenchymal Disease?
Renal parenchyma refers to the functional tissue of the kidneys responsible for filtering waste materials, regulating electrolyte balance, and maintaining fluid equilibrium within the body. Renal parenchymal disease refers to various pathological conditions affecting this essential tissue. The two primary components of the renal parenchyma are the nephrons and the collecting system.

The nephrons are microscopic structures responsible for filtration, reabsorption, and secretion, while the collecting system consists of tubules that collect and transport urine from the nephrons to the renal pelvis. Damage to any part of the renal parenchyma can disrupt kidney function and contribute to the development of renal parenchymal disease.
Causes of Renal Parenchymal Disease
Renal parenchymal disease can arise from various factors, including:
- Hypertension: Uncontrolled high blood pressure which is Hypertension can lead to damage and scarring of the renal parenchyma over time.
- Diabetes: Prolonged uncontrolled diabetes can cause diabetic nephropathy, a common cause of renal parenchymal disease.
- Infections: Chronic or recurring kidney infections, such as pyelonephritis, can lead to renal scarring and parenchymal damage.
- Autoimmune Diseases: Conditions like lupus, vasculitis, and IgA nephropathy can result in inflammation and injury to the renal parenchyma.
- Congenital Abnormalities: Structural defects present at birth, such as polycystic kidney disease, can affect the renal parenchyma and impair kidney function.
- Obstruction: Conditions causing urinary tract obstruction, such as kidney stones or tumours, can lead to renal parenchymal damage if left untreated.
- Medications and Toxins: Certain medications and toxins, including non-steroidal anti-inflammatory drugs (NSAIDs), some antibiotics, and heavy metals, can cause renal parenchymal disease when used in excessive amounts or over a prolonged period.
- Glomerulonephritis: This condition involves inflammation and damage to the glomeruli, the tiny filters within the kidneys. If left untreated, glomerulonephritis can progress to renal parenchymal disease.
- Vascular Disorders: Conditions affecting the blood vessels within the kidneys, such as renal artery stenosis or thrombosis, can impair blood flow and lead to renal parenchymal damage.
- Systemic Diseases: Certain systemic conditions, including systemic lupus erythematosus, vasculitis, and amyloidosis, can affect multiple organs, including the kidneys, leading to renal parenchymal disease.
Symptoms and Clinical Presentation
The symptoms of renal parenchymal disease can vary depending on the underlying cause and the extent of kidney damage. In the early stages, individuals may not experience any noticeable symptoms.
However, as the disease progresses, the following signs and symptoms may manifest:
- Changes in Urinary Patterns: This can include increased frequency of urination, particularly during the night (nocturia), decreased urine output, blood in the urine (hematuria), or foamy urine due to excess protein.
- Edema: Fluid retention and swelling commonly observed in the ankles, legs, and around the eyes.
- Hypertension: High blood pressure can cause or result in renal parenchymal disease.
- Fatigue and Weakness: Generalized tiredness and reduced energy levels.
- Persistent Back Pain: This is a dull or aching pain in the lower back, typically on one side.
- Abdominal Discomfort: Pain or discomfort in the abdominal region, often associated with underlying conditions like polycystic kidney disease.
- Electrolyte Imbalance: Imbalances in electrolyte levels, such as high potassium (hyperkalemia) or low calcium (hypocalcemia), can occur due to impaired kidney function.
It is important to note that these symptoms are not exclusive to renal parenchymal disease and can overlap with other kidney-related or systemic conditions. Proper medical evaluation and diagnostic tests are necessary to determine the underlying cause of these symptoms.
Diagnosis and Evaluation
Diagnosing renal parenchymal disease involves a comprehensive evaluation that combines medical history, physical examination, laboratory tests, imaging techniques, and, in some cases, kidney biopsy. The following are the main components of the diagnostic process:
Medical History and Physical Examination:
The healthcare provider will inquire about the individual’s symptoms, medical history, family history of kidney disease, and any known risk factors. A physical examination may also assess signs such as edema, high blood pressure, or abdominal tenderness.
Laboratory Tests:
Several laboratory tests can provide valuable information about kidney function and help diagnose renal parenchymal disease. These tests may include:
- Urine Analysis: This test evaluates the presence of blood, protein, and other abnormalities in the urine.
- Blood Tests: Measurements of creatinine, blood urea nitrogen (BUN), and electrolyte levels (sodium, potassium, calcium, etc.) can provide insights into kidney function and overall health.
- Glomerular Filtration Rate (GFR): GFR is a crucial indicator of kidney function and is often estimated using equations that consider age, gender, race, and serum creatinine levels.
- Autoimmune Markers: Blood tests may detect autoimmune markers, such as antinuclear antibodies (ANA) or anti-dsDNA antibodies, to assess if the autoimmune-related renal parenchymal disease is present.
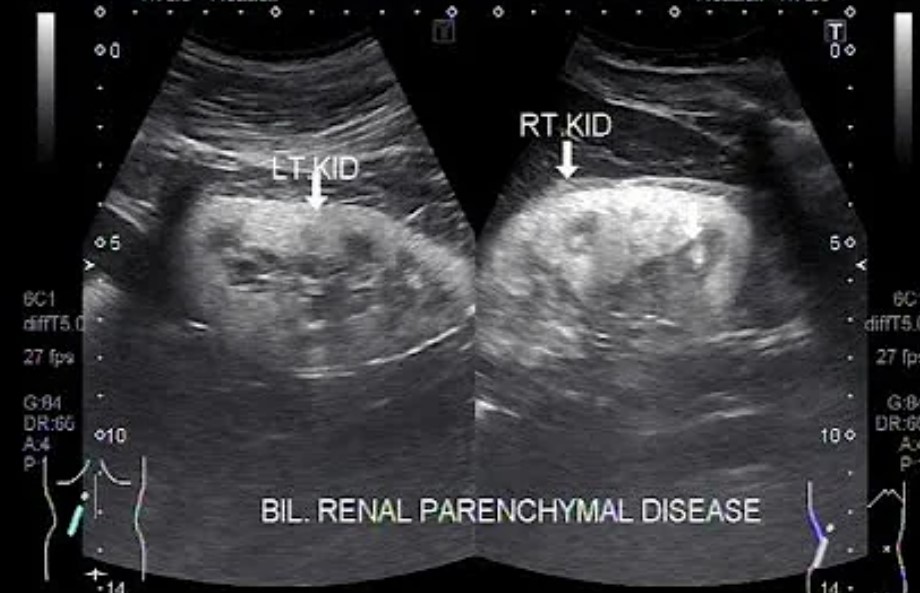
Imaging Techniques:
Imaging studies play a crucial role in evaluating the structure and function of the kidneys. The following imaging techniques may be employed:
- Ultrasound: This non-invasive procedure uses sound waves to create images of the kidneys. It can help detect abnormalities like cysts, tumors, or obstructions.
- CT Scan: A computed tomography (CT) scan provides detailed cross-sectional images of the kidneys, allowing the visualization of renal structures and identification of abnormalities.
- MRI: Magnetic resonance imaging (MRI) utilizes powerful magnets and radio waves to generate highly detailed images of the kidneys. It can provide information about blood flow and tissue characteristics and detect structural abnormalities.
- Renal Scintigraphy: This nuclear medicine imaging technique involves injecting a small amount of a radioactive substance taken up by the kidneys. It helps assess kidney function and blood flow and detect any abnormalities.
Kidney Biopsy:
A kidney biopsy may be recommended when the underlying cause remains unclear or if a specific diagnosis is required. This procedure involves obtaining a small sample of kidney tissue for microscopic examination. A biopsy can provide information about the type and severity of renal parenchymal disease and guide treatment decisions.
Classification and Types of Renal Parenchymal Disease
Renal parenchymal disease encompasses a wide range of conditions affecting the functional tissue of the kidneys. These conditions can be broadly classified into the following categories:
Glomerular Diseases:
Glomerular diseases primarily affect the glomeruli, the kidney’s filtering units. They include:
- IgA Nephropathy: IgA nephropathy (nuh-FROP-uh-thee), also known as Berger’s disease, is a kidney disease that occurs when an antibody called immunoglobulin A (IgA) in the glomeruli, causing inflammation and kidney damage.
- Membranous Nephropathy: In this condition, immune complexes accumulate in the glomerular membrane, leading to thickening and poor filtration.
- Focal Segmental Glomerulosclerosis (FSGS): FSGS involves scarring and sclerosis in specific segments of the glomeruli, resulting in proteinuria and reduced kidney function.
- Minimal Change Disease (MCD): MCD is characterized by normal-appearing glomeruli under a microscope. It is a common cause of nephrotic syndrome in children.
- Lupus Nephritis: A complication of systemic lupus erythematosus (SLE), where the immune system mistakenly attacks the kidneys, leading to inflammation and damage.
Tubular Interstitial Diseases:
Tubular interstitial diseases affect the tubules and interstitial tissue of the kidneys. Examples include:
- Acute Tubular Necrosis (ATN): Often caused by ischemia or toxic injury, ATN results in the death of tubular cells and subsequent kidney function impairment.
- Drug-Induced Nephropathy: Certain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics, and chemotherapeutic agents, can cause tubular interstitial damage.
- Chronic Tubulointerstitial Nephritis: Characterized by chronic inflammation and fibrosis of the tubules and interstitial tissue, often due to prolonged infections, autoimmune conditions, or exposure to toxins.
Vascular Diseases:
Vascular diseases affect the blood vessels within the kidneys and include:
- Renal Artery Stenosis: Narrowing of the renal artery, leading to reduced blood flow to the kidneys.
- Thrombotic Microangiopathy: Conditions such as hemolytic uremic syndrome (HUS) or thrombotic thrombocytopenic purpura (TTP) that cause clot formation in the kidneys’ tiny blood vessels, impairing blood flow and leading to renal parenchymal damage.
- Renal Vasculitis: Inflammation of the blood vessels in the kidneys, often associated with autoimmune disorders such as granulomatosis with polyangiitis (GPA) or microscopic polyangiitis (MPA).
Cystic Diseases:
Cystic diseases involve the formation of fluid-filled sacs (cysts) within the kidneys. Examples include:
- Polycystic Kidney Disease (PKD): Inherited conditions characterized by the development of numerous cysts in the kidneys, leading to progressive enlargement and eventual loss of kidney function.
- Medullary Cystic Kidney Disease: A rare genetic disorder that causes the formation of cysts in the medullary region of the kidneys, leading to impaired tubular function.
Genetic and Congenital Disorders:
Certain genetic and congenital conditions can affect the renal parenchyma, including:
- Alport Syndrome: A genetic disorder characterized by abnormalities in the glomerular basement membrane, leading to progressive kidney damage.
- Congenital Nephrotic Syndrome: A rare condition where infants are born with nephrotic syndrome, characterized by excessive protein loss in the urine and impaired kidney function.
- Renal Dysplasia: Abnormal development of the renal parenchyma during fetal development, leading to structural and functional kidney abnormalities.
Treatment Approaches
Treating renal parenchymal disease aims to manage the underlying cause, slow down the progression of kidney damage, alleviate symptoms, and preserve kidney function. The treatment approach may vary depending on the specific condition and its severity. The following treatment options may be considered:
Medications and Lifestyle Modifications:
- Blood Pressure Control: Hypertension is a common complication of renal parenchymal disease. Medications such as angiotensin-converting enzyme inhibitors (ACE inhibitors) or angiotensin receptor blockers (ARBs) may be prescribed to help control blood pressure and protect kidney function.
- Immunosuppressive Therapy: In cases where autoimmune or glomerular diseases are the underlying cause, medications that suppress the immune system, such as corticosteroids or immunosuppressants, may be prescribed to reduce inflammation and slow down the progression of kidney damage.
- Diuretics: Diuretic medications may be prescribed to help manage fluid retention and reduce edema.
- Treatment of Underlying Infections: If chronic or recurring infections cause renal parenchymal disease, antibiotic treatment is necessary to control the condition and prevent further kidney damage.
- Blood Sugar Control: For individuals with diabetes-related renal parenchymal disease, maintaining reasonable blood sugar control is crucial to slow down the progression of kidney damage.
- Dietary Modifications: A diet low in sodium, protein, and phosphorus may be recommended to manage symptoms and reduce the kidney workload.
Dialysis:
Dialysis may be required in advanced stages of renal parenchymal disease when kidney function is significantly impaired. Dialysis is a medical procedure that helps remove waste products and excess fluid from the blood when the kidneys cannot perform this function adequately. There are two main types of dialysis: hemodialysis, which uses a machine to filter the blood, and peritoneal dialysis, which uses the lining of the abdominal cavity as a filter. The choice of dialysis modality depends on various factors and is determined in consultation with the healthcare team.
Kidney Transplantation:
Kidney transplantation is the treatment of choice for individuals with end-stage renal disease (ESRD) due to renal parenchymal disease. A kidney transplant involves replacing the diseased kidney with a healthy kidney from a living or deceased donor. Kidney transplantation offers the potential for improved quality of life and long-term kidney function compared to dialysis. However, it requires careful evaluation, matching, and lifelong immunosuppressive medications to prevent organ rejection.
Prevention and Management Strategies
While not all cases of renal parenchymal disease can be prevented, adopting specific strategies can help reduce the risk or delay the progression of kidney damage. Consider the following preventive and management measures:
- Manage Underlying Health Conditions: Effectively manage conditions such as hypertension and diabetes through regular medical care, medication adherence, and lifestyle modifications. Maintaining optimal control of these conditions can significantly reduce the risk of renal parenchymal disease.
- Healthy Lifestyle: Adopt a healthy lifestyle that includes regular exercise, a balanced diet, and weight management. This can help prevent or manage conditions such as obesity, which can contribute to kidney damage.
- Stay Hydrated: Drink an adequate amount of water to maintain proper hydration. Sufficient hydration promotes kidney function and helps prevent the formation of kidney stones.
- Avoid Nephrotoxic Substances: Minimize exposure to substances that can harm the kidneys, such as excessive use of over-the-counter pain medications (NSAIDs), illegal drugs, and environmental toxins.
- Regular Check-ups: Schedule regular check-ups with your healthcare provider to monitor kidney function and detect any signs of renal parenchymal disease at an early stage.
- Genetic Counseling: If you have a family history of kidney disease, consider genetic counseling to assess your risk and understand preventive measures.
- Smoking Cessation: Quit smoking if you are a smoker. Smoking can worsen kidney damage and increase the risk of kidney disease progression.
Living with Renal Parenchymal Disease
Living with renal parenchymal disease requires proactive management and lifestyle adjustments to maintain kidney health and overall well-being. Consider the following tips for individuals with renal parenchymal disease:
- Follow Treatment Plan: Adhere to the prescribed treatment plan, including medications, dietary restrictions, and lifestyle modifications. This will help manage symptoms, slow disease progression, and preserve kidney function.
- Regular Monitoring: Stay proactive in monitoring kidney function by attending regular check-ups and follow-up appointments with your healthcare provider. Regular monitoring allows for timely adjustments to the treatment plan and helps identify any complications or changes in kidney function.
- Supportive Care: Seek support from healthcare professionals, such as nephrologists, dieticians, and counselors specializing in kidney health. They can provide guidance, education, and emotional support throughout your journey.
- Healthy Diet: Follow a kidney-friendly diet as your healthcare provider or dietitian recommends. This may include limiting sodium, phosphorus, and protein intake while ensuring adequate information on essential nutrients.
- Hydration: Maintain proper hydration by drinking an appropriate amount of water unless advised otherwise by your healthcare provider.
- Emotional Well-being: Manage stress and seek emotional support to cope with the challenges of living with renal parenchymal disease. Consider joining support groups or seeking counseling to connect with others who understand your experiences.
- Lifestyle Modifications: Make necessary lifestyle modifications, such as regular exercise, weight management, and avoiding smoking or excessive alcohol consumption, to support overall kidney health and minimize risk factors.
Research and Advancements
Ongoing research and advancements in renal parenchymal disease continue to contribute to a better understanding of the condition and the development of improved diagnostic techniques and treatment options. Some areas of research and advancements include:
- Biomarkers: Researchers are exploring using biomarkers to detect early signs of renal parenchymal disease, predict disease progression, and monitor treatment response. Biomarkers may aid in early diagnosis and personalized treatment approaches.
- Precision Medicine: Advancements in genetic and molecular research are paving the way for personalized medicine approaches. Understanding genetic variations and disease mechanisms can help tailor treatment plans and interventions specific to each patient’s needs.
- Regenerative Medicine: The field of regenerative medicine holds promise for kidney regeneration and repair. Researchers are investigating stem cell therapies, tissue engineering, and other regenerative approaches to restore damaged renal parenchyma and improve kidney function.
- Novel Therapies: Innovative therapeutic strategies are being explored, including targeted immunotherapies, gene therapies, and novel drug formulations. These advancements improve treatment outcomes, slow disease progression, and minimize adverse effects.
- Artificial Intelligence (AI) and Machine Learning: AI algorithms and machine learning techniques are being applied to enhance diagnostic accuracy, predict disease outcomes, and optimize treatment decisions in renal parenchymal disease. These technologies have the potential to improve clinical decision-making and patient care.
- Telemedicine and Remote Monitoring: Telemedicine platforms and remote monitoring technologies are increasingly utilized to provide virtual care and remotely monitor patients with renal parenchymal disease. This approach enhances access to healthcare, facilitates regular follow-ups, and improves patient outcomes, particularly for individuals in rural or underserved areas.
Conclusion
Renal parenchymal disease encompasses various conditions that affect the functional tissue of the kidneys, leading to impaired kidney function and potentially progressing to chronic kidney disease or end-stage renal disease. Understanding the causes, symptoms, diagnosis, and treatment options is essential for healthcare professionals and individuals concerned about kidney health.
Early detection, management of underlying conditions, and adherence to prescribed treatments are crucial in slowing disease progression and preserving kidney function. Lifestyle modifications, such as adopting a healthy diet, staying hydrated, and maintaining a physically active lifestyle, can further support kidney health.
Advancements in research, including biomarkers, precision medicine, regenerative medicine, and novel therapies, offer hope for improved diagnostics, personalized treatments, and potential kidney regeneration in the future.
By staying proactive, seeking medical support, and adopting a holistic approach to kidney health, individuals with renal parenchymal disease can optimize their well-being and improve long-term outcomes.
Reference
- National Kidney Foundation (NKF): https://www.kidney.org/
- American Kidney Fund (AKF): https://www.kidneyfund.org/
- Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/kidneydisease/
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): https://www.niddk.nih.gov/
- PubMed: https://pubmed.ncbi.nlm.nih.gov/ (for accessing scientific research articles)