Diabetic Wound Care
Diabetes is a chronic metabolic disorder characterized by high blood sugar levels, which can lead to various complications. One of the most significant complications affecting individuals with diabetes is the development of diabetic wounds. Diabetic wounds are slow-healing and prone to infections, posing a significant challenge in their treatment and management. This article aims to provide a comprehensive guide on diabetic wound care, focusing on strategies to promote effective treatment.
Diabetic Wound Care
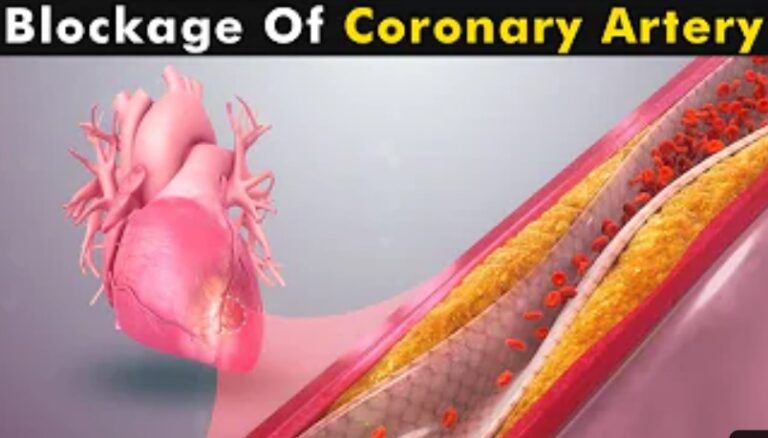
Diabetic wounds are a common complication of diabetes and can be a significant challenge to treat due to their slow healing and high risk of infection. The underlying cause of diabetic wounds is the combination of peripheral neuropathy and poor circulation, which leads to a reduced ability to feel pain and impaired blood flow to the affected area. This combination can result in minor cuts, blisters, or sores that can quickly become infected and lead to more severe wounds.

Understanding Diabetic Wounds
Diabetic wounds occur in the lower extremities, especially the feet, due to the high pressure and shear forces on these areas during everyday activities such as walking or standing. The reduced sensation in the feet due to peripheral neuropathy makes it difficult for individuals with diabetes to recognize and manage injuries early on, leading to delays in treatment and an increased risk of complications.
Early signs of diabetic wounds include redness, swelling, warmth, and drainage, which can quickly progress to more severe symptoms such as necrosis and deep ulcers if left untreated. In some cases, severe diabetic wounds can lead to amputation, highlighting the importance of prompt and effective wound care.
Managing diabetic wounds requires a holistic approach, considering the patient’s overall health and comorbidities, including glycemic control and vascular status. Effective treatment involves assessing the wound’s size, depth, location, and presence of infection.
Proper wound cleaning and debridement are essential to remove debris and bacteria and promote healthy tissue growth. Infection control through appropriate wound dressings and antimicrobial agents is crucial to prevent and treat infections. Moist wound healing through appropriate dressings is also important to create an optimal environment for wound healing and prevent scarring.
Offloading techniques, such as special footwear or pressure-relieving devices, are necessary to reduce pressure on the wound and promote healing. Advanced therapies, such as negative pressure wound therapy, growth factors and bioengineered tissues, and hyperbaric oxygen therapy, may also enhance healing outcomes.
Understanding the underlying causes and early signs of diabetic wounds is crucial in promoting effective treatment and preventing complications. A multidisciplinary approach that considers the patient’s overall health, wound assessment, infection control, moisture management, offloading, and advanced therapies can significantly improve healing outcomes and reduce the risk of complications associated with diabetic wounds.
Importance of Wound Assessment
Wound assessment plays a crucial role in effectively managing and treating diabetic wounds. It involves systematically evaluating the wound’s characteristics and assessing the patient’s overall health and potential underlying factors contributing to impaired wound healing. Here are some reasons why wound assessment is essential:
- Accurate Diagnosis: Wound assessment allows healthcare professionals to diagnose the type and severity of the wound accurately. This information is vital in determining the appropriate treatment plan and interventions. Different types of diabetic wounds, such as neuropathic or ischemic ulcers, require specific management strategies tailored to their unique characteristics.
- Monitoring Healing Progress: Regular wound assessments enable healthcare providers to track the progress of wound healing over time. Healthcare professionals can identify improvements or potential complications by documenting wound measurements, such as size, depth, and appearance. Monitoring healing progress helps determine if the current treatment plan is effective or if adjustments are necessary.
- Identifying Infection: Diabetic wounds are particularly susceptible to infections, which can significantly impede healing. Wound assessment identifies signs and symptoms of infection, such as increased redness, swelling, warmth, purulent drainage, or an unpleasant odor. Prompt recognition of infection enables healthcare professionals to initiate appropriate antimicrobial therapy and prevent the spread of infection.
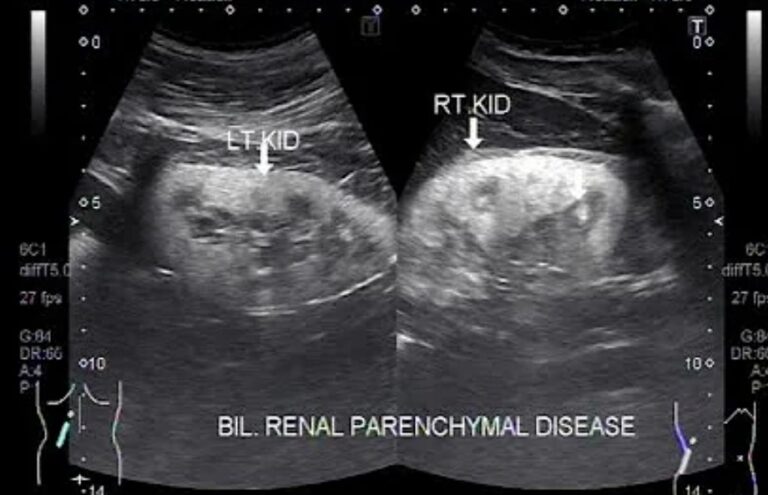
- Evaluating Underlying Factors: Wound assessment considers various factors contributing to impaired wound healing, such as poor glycemic control, compromised vascular supply, or comorbidities like peripheral neuropathy. Understanding these underlying factors helps healthcare providers address the root causes and implement interventions that promote optimal healing.
- Tailoring Treatment Plans: Based on the findings of the wound assessment, healthcare professionals can develop personalized treatment plans for each patient. This may include selecting appropriate wound dressings, debridement techniques, offloading strategies, or considering advanced therapies. Individualized treatment plans increase the likelihood of successful wound healing and reduce the risk of complications.
Wound assessment is essential in diabetic wound care as it aids in accurate diagnosis, monitors healing progress, identifies infections, evaluates underlying factors, and allows for tailored treatment plans. By conducting thorough and regular wound assessments, healthcare professionals can provide effective care, optimize healing outcomes, and prevent further complications in individuals with diabetic wounds.
Principles of Diabetic Wound Care
Effective diabetic wound care involves a comprehensive approach that addresses various principles to promote optimal wound healing. Here are the key principles of diabetic wound care:
- Wound Cleaning and Debridement: Proper wound cleaning is essential to remove debris, bacteria, and necrotic tissue from the wound bed. A mild, non-irritating cleanser and gentle irrigation with sterile saline or wound cleansers help maintain a clean wound environment. Debridement, removing non-viable tissue, promotes wound healing by facilitating healthy tissue growth. This can be accomplished through sharp debridement, enzymatic debridement, autolytic debridement, or mechanical debridement.
- Infection Control: Diabetic wounds are prone to infections, significantly impeding healing. Appropriate infection control measures are crucial to prevent and treat infections. This includes selecting the appropriate wound dressings with antimicrobial properties, such as silver dressings, and using topical antimicrobial agents when necessary. Systemic antibiotics may be prescribed in cases of suspected or confirmed infection.
- Moist Wound Healing: Creating a moist wound environment promotes optimal healing. This can be achieved using appropriate wound dressings that maintain moisture, such as hydrogels, hydrocolloids, or foam dressings. Moist wound healing enhances reepithelialization, reduces pain, and prevents scarring. It also supports the migration of cells necessary for tissue regeneration.
- Offloading and Pressure Redistribution: In diabetic foot ulcers, pressure and shear forces contribute to wound development and delayed healing. Offloading techniques reduce pressure on the wound site, allowing optimal healing conditions. This may involve specialized footwear, such as diabetic shoes or custom orthotics, as well as pressure-relieving devices like foam pads or offloading boots. Offloading helps alleviate pressure and shear forces, promoting improved blood flow and tissue perfusion to the wound site.
- Blood Sugar Control: Maintaining good glycemic control is essential for diabetic wound healing. High blood sugar levels can impair the immune response, delay wound healing, and increase the risk of infections. Patients with diabetes should be encouraged to manage their blood sugar levels through diet, medication, and regular monitoring. Collaborating with a healthcare provider specializing in diabetes management can help patients achieve optimal glycemic control.
- Nutritional Support: Proper nutrition is vital for wound healing. Diabetic individuals should be educated about the importance of a balanced diet rich in nutrients, including proteins, vitamins (especially C and zinc), and minerals. Adequate nutrition supports collagen synthesis, angiogenesis, and the overall healing process.
By following these principles, healthcare professionals can promote effective wound healing, reduce the risk of complications, and improve the overall outcomes of diabetic wound care. Individualized treatment plans should be developed based on each patient’s wound’s specific characteristics and needs. Regular reassessment and adjustments to the treatment plan may be necessary to ensure optimal wound healing.
Advanced Therapies in Diabetic Wound Care
In addition to the basic principles of diabetic wound care, several advanced therapies are available that can significantly enhance the healing process and improve outcomes. These therapies are often considered when standard wound care approaches have not yielded satisfactory results. Here are some advanced therapies commonly used in diabetic wound care:
- Negative Pressure Wound Therapy (NPWT): Negative pressure wound therapy involves the application of controlled negative pressure to the wound bed using a specialized dressing and a vacuum-assisted device. NPWT promotes wound healing through several mechanisms, including improved blood flow, excess fluid removal, and granulation tissue formation. It also helps to reduce edema, increase oxygenation, and enhance the formation of new blood vessels.
- Growth Factors and Bioengineered Tissues: Growth factors and bioengineered tissues promote tissue regeneration and wound healing. Growth factors, such as platelet-derived growth factor (PDGF) or epidermal growth factor (EGF), can be applied topically or delivered via injections to stimulate cell proliferation and migration, angiogenesis, and collagen synthesis. Bioengineered tissues, such as skin substitutes or dermal matrices, provide a scaffold for cell growth and help replace lost or damaged tissue.
- Hyperbaric Oxygen Therapy (HBOT): Hyperbaric oxygen therapy involves exposing the patient to 100% oxygen at higher atmospheric pressure in a hyperbaric chamber. This therapy increases the oxygen concentration in the blood and tissues, promoting angiogenesis, enhancing antibacterial activity, and supporting healing. HBOT particularly benefits diabetic wounds with compromised blood flow, such as ischemic ulcers or non-healing surgical wounds.
- Electrical Stimulation: Electrical stimulation therapy applies low-level electrical currents to the wound site to promote healing. This therapy can help improve blood flow, enhance cell migration and proliferation, and stimulate the production of growth factors. Electrical stimulation is particularly useful for chronic, non-healing wounds, including diabetic ulcers.
- Ultrasonic Therapy: Ultrasonic therapy utilizes high-frequency sound waves to promote wound healing. The mechanical vibrations generated by the ultrasound waves help debride the wound by breaking down non-viable tissue and bacteria. It also enhances cellular activity, increases collagen synthesis, and improves the effectiveness of topical treatments.
- Oxygen-Generating Wound Dressings: Oxygen-generating wound dressings are innovative dressings that release oxygen directly to the wound bed. These dressings contain materials that react with wound exudate or moisture to produce and deliver oxygen to the wound site. The oxygen helps create an optimal healing environment, supports aerobic bacterial control, and promotes tissue regeneration.
It is important to note that advanced therapies in diabetic wound care should be based on a thorough assessment of the wound and individual patient factors. Healthcare professionals should consider the benefits, risks, and suitability of these therapies for each patient, considering their overall health and specific wound characteristics.
While these advanced therapies can be highly effective, they are often utilized with the basic principles of wound care, including wound cleaning, infection control, moisture management, offloading, and optimizing blood sugar control. A multidisciplinary approach involving wound care specialists, podiatrists, surgeons, and other healthcare professionals is crucial to determine the most appropriate advanced therapy and ensure comprehensive wound management.
Prevention and Patient Education
Preventing diabetic wounds is paramount to reducing the risk of complications and improving overall patient outcomes. Patient education is crucial in empowering individuals with diabetes to take proactive measures to prevent wounds and effectively manage their condition. Here are key aspects of prevention and patient education in diabetic wound care:
- Foot Care Education: Educating patients about proper foot care is essential, as the feet are particularly vulnerable to diabetic wounds. Patients should be encouraged to perform daily foot inspections, checking for any cuts, blisters, or changes in skin color. They should be advised to keep their feet clean and dry, trim their nails carefully, and wear appropriate footwear that fits well and provides adequate support and protection.
- Glycemic Control: Emphasizing the importance of maintaining good glycemic control is crucial in preventing diabetic wounds. Patients should be educated on the significance of monitoring and managing their blood sugar levels through self-monitoring, adhering to prescribed medications, following a healthy diet, and engaging in regular physical activity. Keeping blood sugar levels within target ranges promotes better wound healing and reduces the risk of complications.
- Lifestyle Modifications: Encouraging patients to adopt a healthy lifestyle is beneficial for overall wound prevention. This includes promoting a balanced diet rich in nutrients, particularly those supporting wound healing, such as proteins, vitamins, and minerals. Regular exercise is also important for improving circulation and maintaining a healthy weight. Additionally, counselling patients on the harmful effects of smoking and encouraging smoking cessation is crucial, as smoking impairs wound healing and increases the risk of complications.
- Risk Factor Awareness: Patients should be educated about the risk factors contributing to diabetic wounds. This includes emphasizing the importance of managing hypertension and dyslipidemia, which can impact wound healing. Patients should also be made aware of the potential consequences of peripheral neuropathy and peripheral arterial disease and the need for regular screening and monitoring of these conditions.
- Regular Follow-up Care: A regular follow-up care plan with healthcare professionals is essential. Patients should be encouraged to attend scheduled appointments to monitor their foot health, assess wound risk, and promptly address any concerns or issues.
By providing comprehensive education on preventive measures and self-care, patients with diabetes can actively participate in their wound prevention and management. Empowered with knowledge, they can make informed decisions, adopt healthier lifestyles, and take necessary steps to minimize the risk of diabetic wounds and their associated complications.
Effective diabetic wound care involves a multidisciplinary approach that combines wound assessment, infection control, moisture management, offloading, and advanced therapies. By following these principles, healthcare professionals can improve healing outcomes and reduce the risk of complications associated with diabetic wounds. Equally important is the focus on prevention and patient education, which empowers individuals